Guillain-Barré Syndrome (GBS) is a rare but serious autoimmune disorder in which the body’s immune system mistakenly attacks the peripheral nervous system, including the nerves that control muscle movement and sensation. While the exact cause of Guillain-Barré Syndrome remains unclear, it often follows infections such as respiratory illnesses, gastrointestinal infections (commonly caused by Campylobacter jejuni bacteria), or, less frequently, viral infections like cytomegalovirus (CMV) and Epstein-Barr virus (EBV). This immune response damages the protective covering (myelin sheath) surrounding the nerves or, in some cases, the nerve fibers themselves, leading to impaired nerve signal transmission.
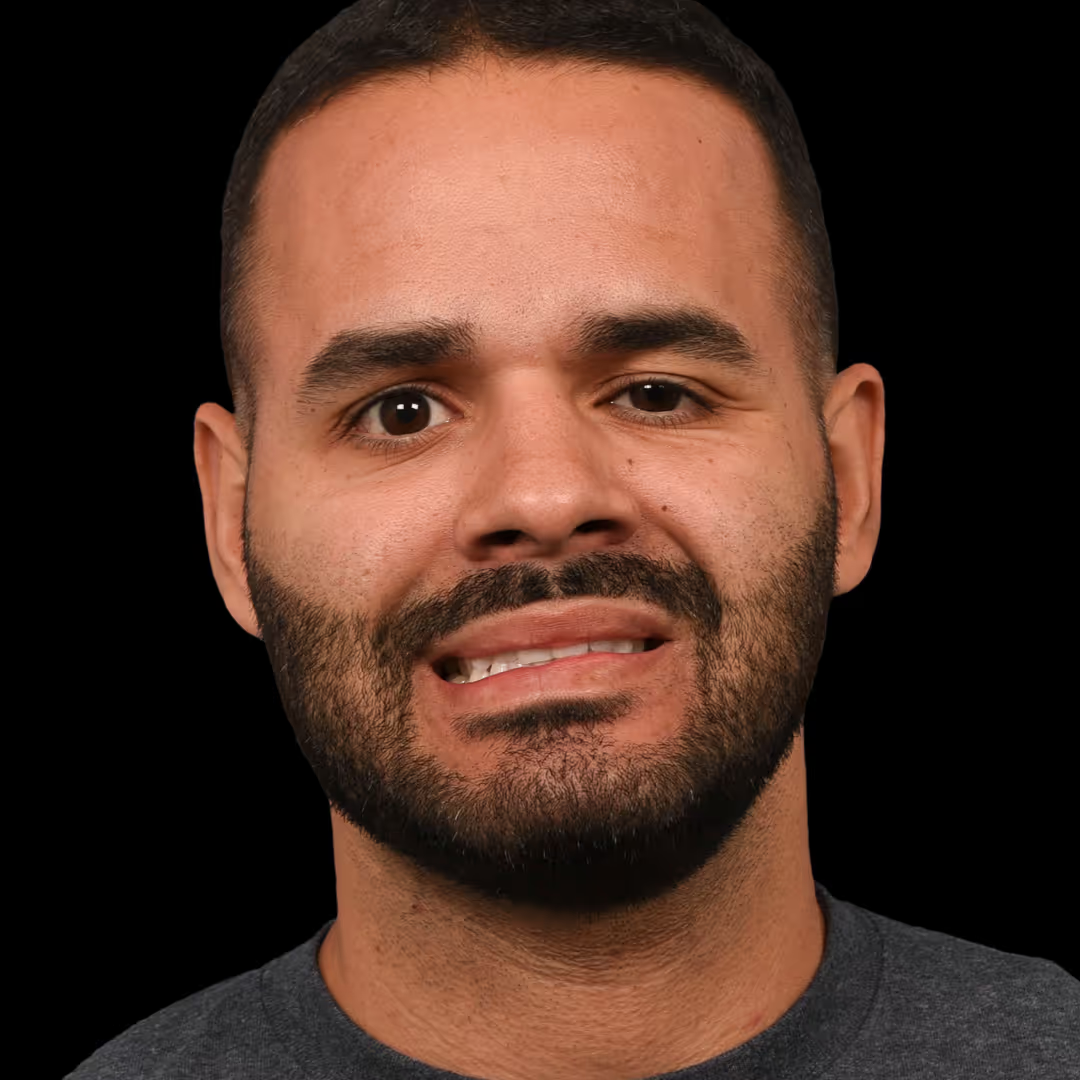
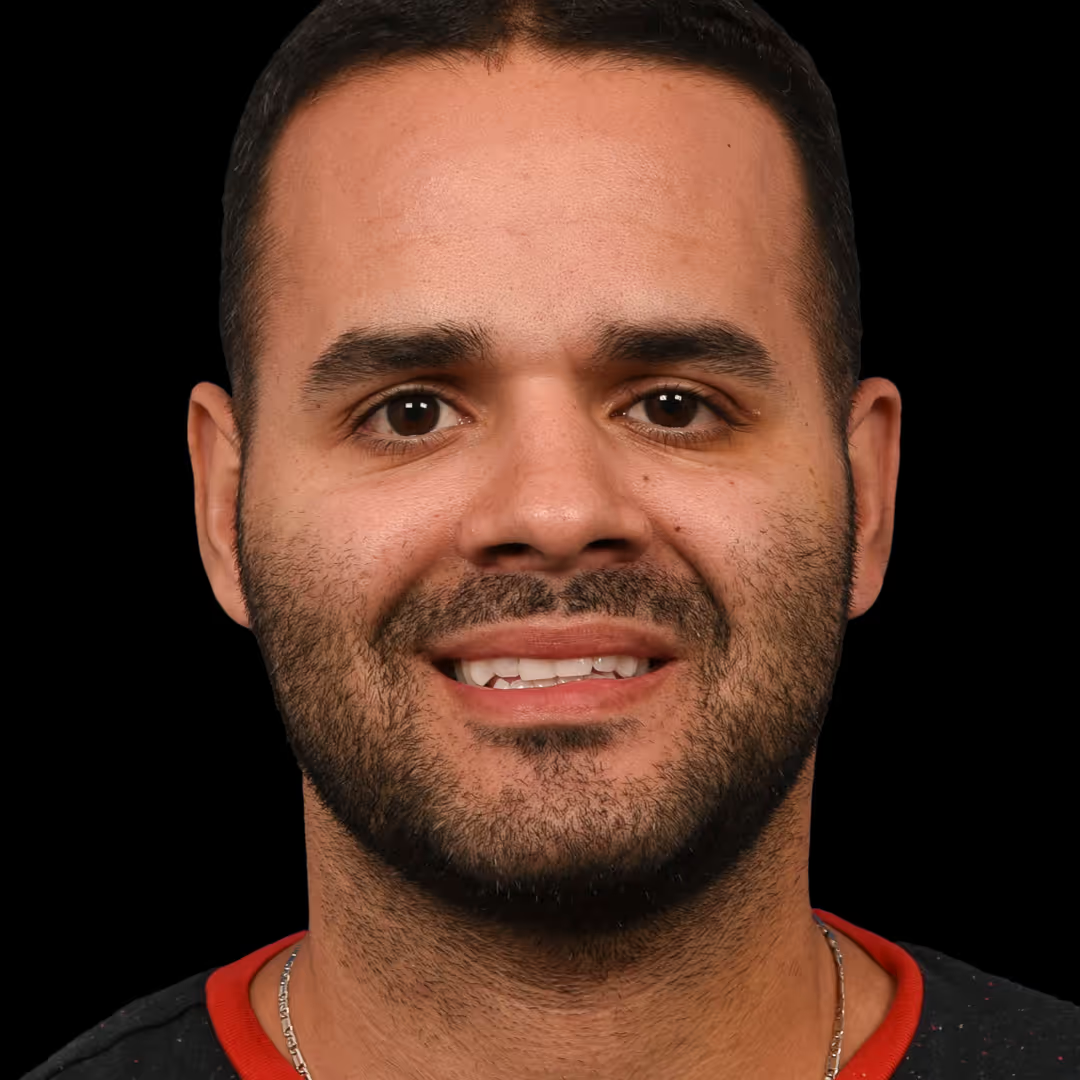
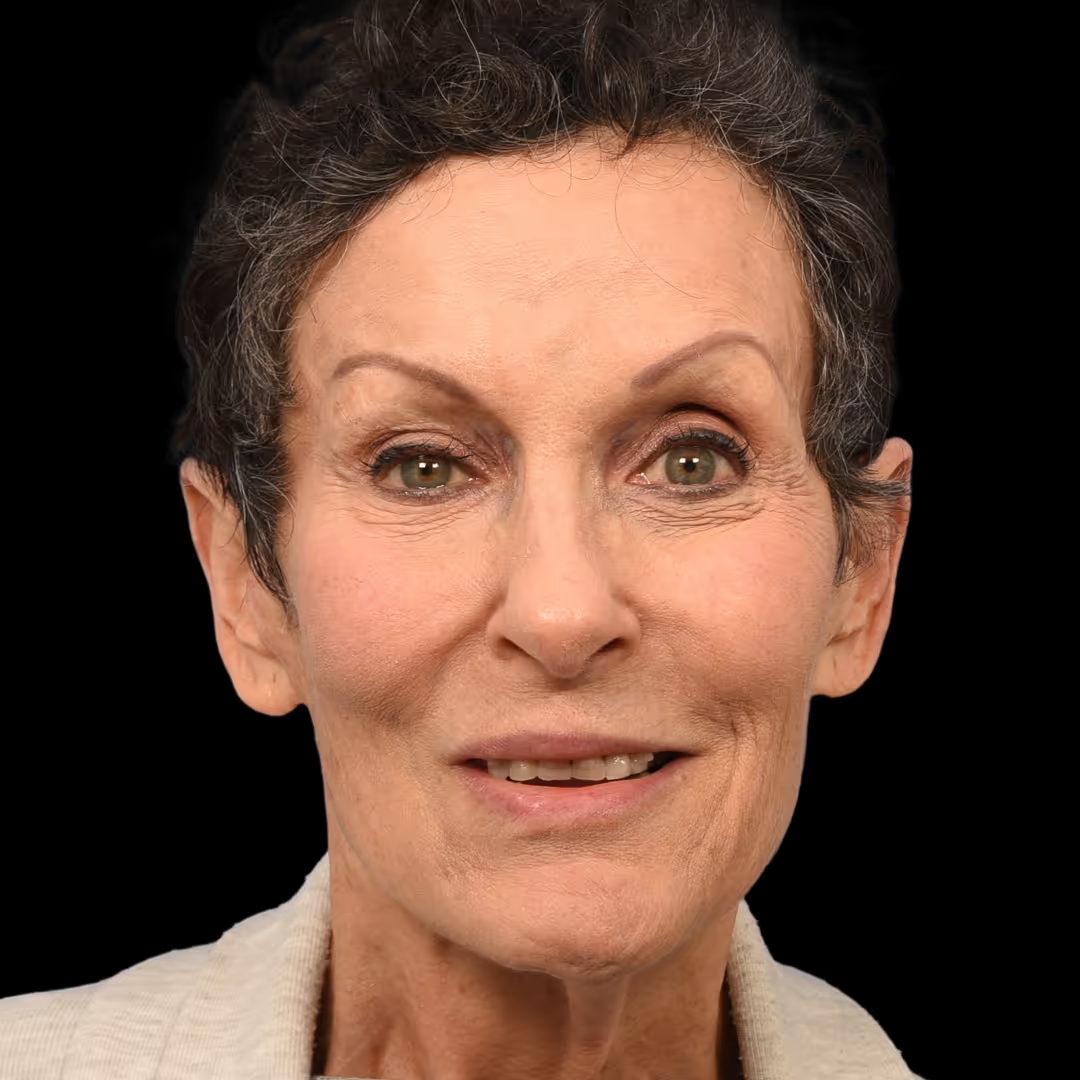
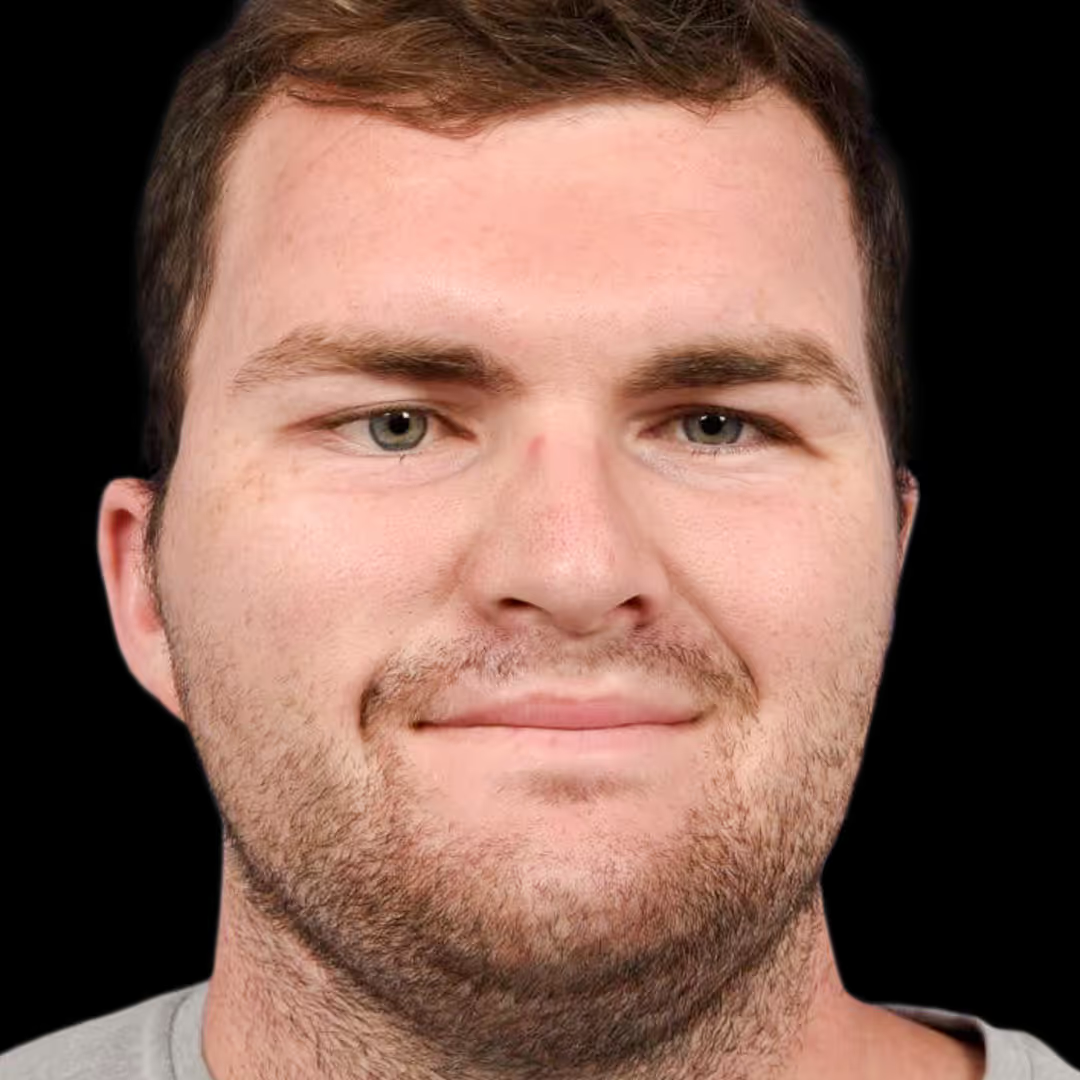
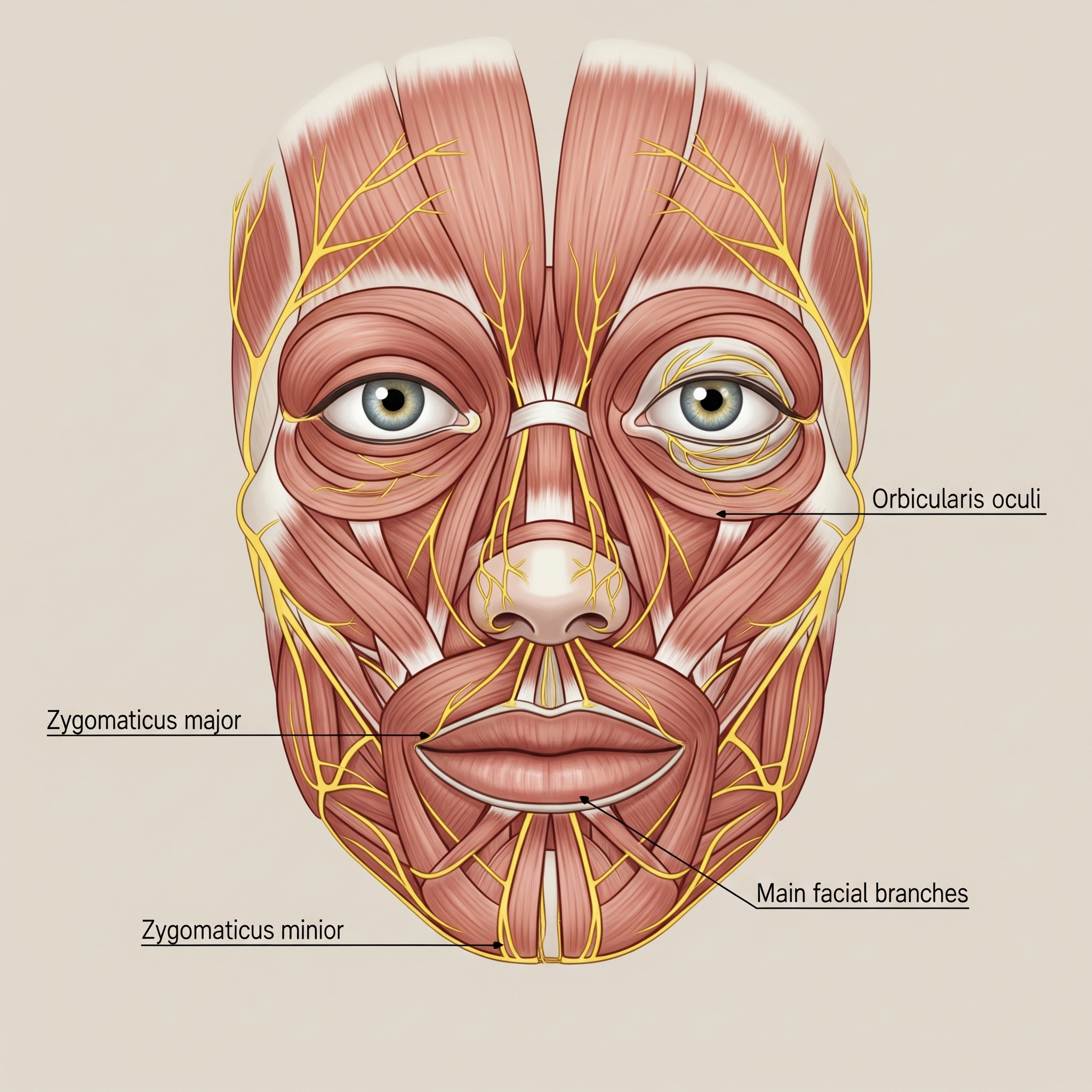
Facial paralysis in Guillain-Barré Syndrome occurs when the immune attack targets the facial nerves, resulting in inflammation and demyelination. This can lead to weakness or paralysis of one or both sides of the face, making it difficult to close the eyes, smile, or make other facial expressions. Facial nerve involvement is common in GBS, occurring in approximately 50% of cases, and can often be mistaken for other causes of facial paralysis, such as Bell’s palsy. However, unlike isolated facial nerve palsies, GBS-related facial paralysis is usually accompanied by other neurological symptoms, such as muscle weakness, numbness, tingling in the extremities, loss of reflexes, and, in severe cases, respiratory difficulties due to involvement of the nerves controlling breathing.
The diagnosis of GBS is typically made based on clinical symptoms, electromyography (EMG) findings, and cerebrospinal fluid analysis, which often shows an increased protein concentration without an elevated white blood cell count. Treatment for Guillain-Barré Syndrome focuses on halting the autoimmune attack through therapies such as intravenous immunoglobulin (IVIG) or plasmapheresis (plasma exchange), which help to reduce immune system activity. Supportive care, including physical therapy and, if needed, respiratory support, is critical to managing symptoms and aiding recovery.
Facial paralysis resulting from GBS generally improves over time as the immune response is controlled and nerve function gradually recovers. However, recovery can be slow, taking weeks to months, and may require rehabilitative therapies to restore strength and function to the affected facial muscles. Synkinesis may occur on one or both sides of the face, often requiring multidisciplinary care involving facial nerve experts, neurologists, and rehabilitation specialists to optimize outcomes and address any residual functional or cosmetic concerns.
(1).png)


















.png)
.png)