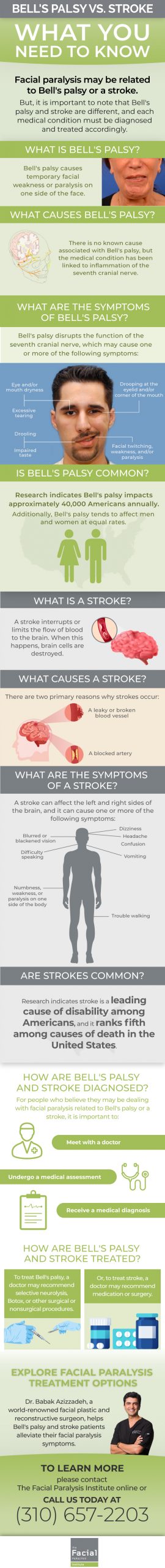
Bell’s palsy and stroke are medical conditions commonly associated with facial paralysis. However, Bell’s palsy and stroke are not identical, and proper diagnosis is key to ensure safe, effective treatment of either condition. To better understand the differences between Bell’s palsy and stroke, let’s examine both conditions in detail.
The Difference Between Bell’s Palsy and Stroke
Bell’s palsy is a form of temporary facial paralysis that affects the seventh cranial nerve; this nerve is located in the skull and travels beneath the ears to muscles on both sides of the face. It causes an interruption in messages between the brain and facial nerves, resulting in facial paralysis or weakness.
When Bell’s palsy occurs, the seventh cranial nerve’s functionality is disrupted. This makes it difficult for an individual to open and close the eyes and smile, frown and make other facial expressions.
Bell’s palsy symptoms range from mild to severe, and they can affect one or both sides of the face. Common Bell’s palsy symptoms include facial twitching and weakness, along with facial paralysis. Additionally, people who experience Bell’s palsy are prone to drooling, eye or mouth dryness, excessive tearing, drooping at the eyelid and corner of the mouth and impaired taste.
Oftentimes, Bell’s palsy symptoms reach their apex within 48 hours of onset. At this point, an individual coping with Bell’s palsy could experience ringing in one or both ears, headache, impaired speech, dizziness and hypersensitivity to sound. This individual could also have difficulty eating or drinking.
Bell’s palsy affects approximately 40,000 Americans annually, according to the National Institute of Neurological Disorders and Stroke (NIH). The condition impacts men and women at equal rates, and people above the age of 60 and under the age of 15 are less susceptible to Bell’s palsy than others.
To date, no known cause of Bell’s palsy has been identified. There is an understanding that Bell’s palsy occurs due to inflammation that affects the seventh cranial nerve, yet research is ongoing to determine the precise cause of this inflammation. Meanwhile, Columbia University Department of Neurology notes that Bell’s palsy symptoms are sometimes associated with a variety of medical conditions, including diabetes, high blood pressure and Lyme disease.
In comparison to Bell’s palsy, stroke is a leading cause of disability and the fifth-ranked cause of death in the United States, American Stroke Association (ASA) states. Stroke refers to a disease that impacts arteries in the brain. It occurs when a blood vessel that transports oxygen and nutrients to the brain is blocked; this blockage happens due to a clot or bursts. In this instance, the brain cannot get the necessary blood and oxygen it needs to function properly, thus resulting in the death of brain cells.
There are three types of strokes: ischemic, hemorrhagic and transient ischemic attack (TIA). An ischemic stroke occurs when a blood vessel that supplies blood and oxygen to the brain is obstructed; this type of stroke accounts for roughly 87% of all strokes, ASA reports. A hemorrhagic stroke takes place when a weakened blood vessel ruptures, which causes blood to accumulate in the brain and compress surrounding brain tissue. ASA points out that hemorrhagic strokes account for about 13% of all strokes. A TIA, also called a mini stroke, refers to a temporary blockage of blood flow to the brain. Although a TIA likely won’t cause permanent damage, it could be a warning sign that a full-blown stroke could occur in the foreseeable future, ASA states.
Ultimately, a stroke can affect both the left and right sides of the brain. If a stroke impacts the left side of the brain, the right side of the body will be affected. In this scenario, a person may experience paralysis on the right side of the body, as well as deal with speech problems and memory loss. Comparatively, if a stroke impacts the right side of the brain, the left side of the body will be affected. And in this instance, an individual may experience paralysis on the left side of the body, along with vision problems and memory loss.
Bell’s Palsy vs Stroke Symptoms
In patients dealing with Bell’s palsy, the seventh cranial nerve becomes inflamed. The nerve’s branches control motor and sensory functions of the cheeks, mouth, eyelids, and tear glands. As such, Bell’s palsy can affect a patient’s ability to salivate, frown, and perform other facial muscle movements relating to these functions.
With Bell’s palsy, facial weakness can occur in a peripheral pattern in which the forehead mouth, eye, and forehead are affected. Bell’s palsy can hinder a patient’s ability to grimace or smile, open or close the eye, and lift or furrow their eyebrow. It can also cause flattening of the nasolabial fold.
During a stroke, a patient experiences an abrupt disruption in the delivery of oxygen and nutrients to the brain. The symptoms of a stroke can appear within minutes of the disruption and vary based on the affected blood vessel and the resulting shortage of oxygen and nutrients in the brain.
A stroke can cause central facial weakness in which only the mouth is affected. But, there may also be times when strokes result in facial weakness that affects the mouth, eye, and forehead. In these cases, other focal neurologic deficits may be present as well.
Proper assessment of a patient’s symptoms is vital in cases where facial weakness has occurred. By undergoing a neurological examination and other testing, patients can find out if they are dealing with Bell’s palsy or stroke.
Bell’s Palsy vs Stroke Assessment
A Bell’s palsy patient can display unilateral facial paralysis that replicates a stroke. The patient can also experience reduced tearing, drooping on the paralyzed side of the face, slurred speech, and other symptoms.
Along with dealing with symptoms commonly associated with Bell’s palsy, a stroke patient can experience dizziness, loss of coordination, changes in vision, and other sensory issues. Most stroke patients can also blink the eyes and furrow the brow.
If patients display symptoms of Bell’s palsy or stroke, an assessment is used to provide an accurate diagnosis. The assessment involves evaluating a patient’s medical history and conducting a physical exam, followed by a neurologic exam.
The neurologic exam lets a doctor examine a patient’s level of consciousness and their ability to perform facial muscle movements. It can include a cranial nerve exam, stroke scale evaluation, and other tests that correspond to a patient’s symptoms.
Following testing, a doctor determines a safe, effective way to help a patient manage their symptoms. The doctor can use the insights to properly diagnose Bell’s palsy or stroke and help a patient achieve long-lasting symptomatic relief.
How Are Bell’s Palsy and Stroke Diagnosed and Treated?
For an individual who displays any signs of Bell’s palsy or stroke, immediate diagnosis and treatment is essential. By meeting with a doctor at the first sign of Bell’s palsy or stroke symptoms, an individual can get the help necessary to address these symptoms.
There are no laboratory tests used to diagnose Bell’s palsy, according to NIH. Instead, a doctor examines a patient to assess any signs of upper and lower facial weakness. A doctor can also perform an electromyography (EMG) to verify if nerve damage is present. If nerve damage is found, a physician uses an EMG to assess the severity of the damage and extent of nerve involvement as well. Moreover, blood tests are sometimes used to diagnose diabetes, infections and other medical problems that occur in conjunction with Bell’s palsy. Or, a magnetic resonance imaging (MRI) or computed tomography (CT) scan can be used to identify structural issues that put pressure on the facial nerve. Other tests can be used as part of a Bell’s palsy diagnosis, too. These tests include a neurologic assessment, hearing test, tearing test and ear, nose and throat evaluation.
ASA states that a doctor performs two types of tests to diagnose a stroke: imaging and blood flow tests. Imaging tests include MRI and CT scans and help a doctor identify the cause of a stroke and location and extent of a brain injury. Blood flow tests like a cerebral angiography allow a doctor to evaluate blood flow through the vessels to detect blockages and assess their size and severity.
Once a doctor diagnoses Bell’s palsy or stroke, a personalized treatment plan is crafted for a patient. For Bell’s palsy, initial treatment usually involves high-dose steroids and antiviral medications. If a Bell’s palsy patient does not respond to this treatment, other treatment options are available, including:
- Selective Neurolysis: Developed by globally recognized facial plastic and reconstructive surgeon Dr. Babak Azizzadeh, selective neurolysis is a surgical procedure that helps Bell’s palsy patients achieve a natural-looking smile.
- Botox: Bell’s palsy patients can receive Botox injections that temporarily restore facial symmetry and improve the facial appearance.
- “Supercharging” Procedure: A “supercharging” or “signal upgrading” surgical procedure helps increase the power of the facial nerve and strengthen weak smile muscles.
Stroke treatment varies based on the type of stroke, ASA states. An ischemic stroke is commonly treated with tissue plasminogen activator – r-tPA, an FDA-approved medication that dissolves a blood clot and improves blood flow to the brain. It can also be treated with an endovascular procedure or a mechanical thrombectomy procedure to remove a blood clot. For a hemorrhagic stroke, an endovascular procedure is sometimes used to stop bleeding. In certain instances, hemorrhagic stroke surgery is performed to secure a blood vessel at the base of an aneurysm, a weak area in a blood vessel that becomes larger due to a stroke. Finally, to treat a TIA, anti-platelet drugs, anticoagulants and thrombolytic agents can be used. An endarterectomy is sometimes recommended to remove fatty deposits on carotid arteries that otherwise increase the risk of stroke. Angioplasty is also used to treat a TIA; this procedure involves the use of a balloon-like device to open a clogged artery and a small wire tube that keeps the artery open.
The Bottom Line on Bell’s Palsy vs Stroke
If a patient displays symptoms of Bell’s palsy or stroke, there is no need to wait to pursue medical treatment. At this time, a doctor can assess a patient to find out if their symptoms are related to Bell’s palsy or stroke. The doctor can then provide the patient with a personalized diagnosis and treatment plan.
Patients who fail to address their Bell’s palsy or stroke symptoms risk long-term health problems. By being proactive in their efforts to manage these symptoms, patients can alleviate facial weakness and other issues before they escalate. These patients can also take the necessary steps to prevent facial paralysis from hampering their ability to smile, frown, and make other natural facial expressions.
Share this Image On Your Site
Schedule a Facial Paralysis Treatment Consultation with Dr. Azizzadeh Today
Facial paralysis is a problem that affects both Bell’s palsy and stroke patients. With help from Dr. Azizzadeh, a Bell’s palsy or stroke patient can quickly and safely address his or her facial paralysis symptoms.
Dr. Azizzadeh is a Harvard-trained facial plastic and reconstructive surgeon with many years of facial paralysis treatment experience. He works closely with each patient to understand his or her facial paralysis symptoms and delivers a custom treatment plan. That way, Dr. Azizzadeh can help Bell’s palsy and stroke patients correct their facial paralysis symptoms.
Dr. Azizzadeh is available to meet with a Bell’s palsy or stroke patient to explore facial paralysis treatment options. To schedule a facial paralysis treatment consultation with Dr. Azizzadeh, please contact us online or call us today at (310) 657-2203.
Request your consultation with Dr. Azizzadeh today
Call us at (310) 657-2203 to schedule an appointment.
Schedule a Consultation