An acoustic neuroma is the most common kind of non-cancerous brain tumor. While acoustic neuromas are not cancerous, they can cause a variety of problems and should be treated by an expert. Dr. Azizzadeh, Director of the Facial Paralysis Institute, treats some of the common side effects of acoustic neuroma—facial paralysis and incomplete eyelid closure -and works with House Ear Institute surgeons in coordinating all aspects of acoustic neuroma care from diagnosis to surgery to post-acute care.
Dr. Azizzadeh is a leader in the field of facial paralysis treatment and has restored facial movement in countless patients. To ensure the best possible outcomes for his patients, Dr. Azizzadeh works alongside some of the top medical professionals in the country when individuals are having difficulty with their facial nerve after acoustic neuroma surgery, including specialist oculoplastic surgeon Guy Massry,MD, and Facial Neuromuscular Retraining Therapist Jackie Diels.
Post-Acoustic Neuroma Surgery
Acoustic neuroma develops in close proximity to the facial nerve, making it possible for the facial nerve to be damaged during acoustic neuroma removal surgery, and sometimes it is even necessary to remove a portion of the facial nerve in order to effectively remove the entire tumor. Dr. Azizzadeh works closely with expert oculoplastic surgeon Dr. Massry and Facial Neuromuscular Retraining Therapist Jackie Diels to help patients recover from acoustic neuroma removal surgery. Through specialized treatment plans tailored to the individual, they combine facial paralysis expertise, skilled eye care, and muscular retraining therapy to help restore normal facial movements in the acoustic neuroma patient.
When is it time to consider facial reanimation after acoustic neuroma surgery?
View Dr. Azizzadeh’s presentation for the Acoustic Neuroma Association on facial paralysis treatment options following acoustic neuroma surgery. Dr. Azizzadeh discusses all of the current facial reanimation treatment options, including the management of partial paralysis and synkinesis.
Acoustic Neuroma Facial Paralysis
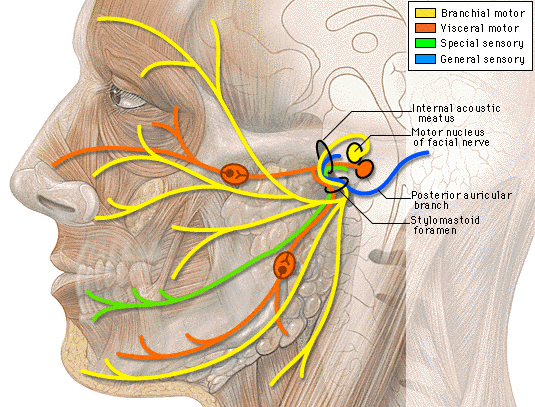
Facial paralysis associated with acoustic neuroma generally occurs as a result of the facial nerve’s proximity to the tumor. Sometimes a section of the facial nerve may need to be removed or manipulated when removing an acoustic neuroma, and, due to the delicate nature of the facial nerve, the residual swelling and damage of the trauma can cause temporary or permanent facial paralysis and synkinesis.
Synkinesis, meaning “simultaneous movement,” is a common occurrence in people with facial palsy. Synkinesis can occur as a result of the abnormal regeneration of the facial nerve after surgery and when the nerve fibers reconnect to the wrong nerve group, it results in undesired facial movements where muscles other than those intended contract. Synkinesis is often treated with Botox injections to relax the hyperactive muscles, but some patients may benefit from surgery.
If a patient does not regain facial movement and/or suffers from severe synkinesis, they may benefit from a nerve transfer surgery. Dr. Azizzadeh is a nerve transfer expert who is highly regarded around the world for his innovative facial paralysis surgery techniques. Depending on your individual case, you may be a candidate for one of the following nerve transfer procedures:
- Hypoglossal-Facial Nerve Transfer
- Masseter-Facial Nerve Transfer
- Gracilis Muscle Transplant
- Temporalis Tendon Transfer
- Surgery for Synkinesis
It is critical that anyone living with permanent facial paralysis caused by acoustic neuroma visit a facial paralysis expert for any treatment. Dr. Azizzadeh uses a multidisciplinary approach to ensure the best possible outcome for all of his facial paralysis procedures and he uses minimally invasive techniques whenever possible. Dr. Azizzadeh’s goal is to put a smile back on the face of all his facial paralysis patients.
Possible Damage and Rehabilitation
For those diagnosed with an acoustic neuroma, there are many aspects of treatment. In this article, Dr. Azizzadeh discusses the nuances of treating an acoustic neuroma while preserving facial nerve function.
Acoustic Neuroma Dizziness
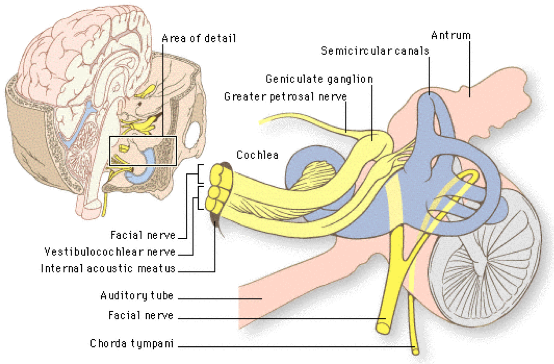
A common effect of acoustic neuroma is dizziness, and it is usually one of the first symptoms of the problem. Vertigo occurs at the onset because the acoustic neuroma starts from the vestibular nerve—the nerve that is responsible for balance. It is common for patients to experience vertigo early on in acoustic neuroma development, but usually as the body adjusts and compensates for the pressure on the vestibular nerve, the patient’s vertigo symptoms will diminish.
Imbalance can progress as the tumor increases in size, while true vertigo subsides. Both conditions—vertigo and imbalance—can present with the symptom of dizziness. The treatment for acoustic neuroma dizziness will depend on the treatment path taken for the tumor itself and some dizziness may remain immediately following acoustic neuroma surgery due to the trauma experienced by nerves during surgery.
Acoustic Neuroma Eye Care
It is fairly common for acoustic neuroma patients to struggle with long-term eye troubles. In fact, about 50% of acoustic neuroma patients have eye discomfort and eye problems such as decreased eyelid function and tear production. These eye problems can lead to eye irritation and a dry, scratchy feeling in the eye due to a lack of protection. It is also very common for patients to use artificial tears to aid in lubrication and prevent dryness. Because proper eyelid function is crucial to the lubrication and protection of the eyeball, Dr. Azizzadeh and Dr. Massry have several methods for restoring some of the eyelid function lost in patients with acoustic neuroma, including:
- Gold Eyelid Weights
- Platinum Chains
- Eyelid Springs
- Tarsorapphy
These procedures can help restore some or all of the ability to close the eyes, which will help keep the eyes protected and prevent eye damage. Dr. Azizzadeh and Dr. Massry use minimally invasive surgical techniques and closes incisions with plastic surgery techniques to reduce the amount of visible scarring.
Dental and Oral Hygiene in Acoustic Neuroma Patients
All tumors come with their own set of unique traits. An acoustic neuroma is a benign growth that can be found on the eighth cranial nerve (also known as the vestibulocochlear nerve). This nerve connects the inner ear to the brain and is comprised of two main components; an auditory portion and the vestibular portion. Acoustic neuromas, also known as vestibular schwannomas, are non-cancerous and have a wide variety of treatment options including surgery, radiation, or observation. When acoustic neuromas become large enough or as a result of surgical treatment or radiation therapy, its function can become altered or compromised leading to a plethora of unpleasant side effects. The most common issues that can affect acoustic neuroma patients include tinnitus, partial or complete deafness, imbalance, headache, numbness and occasionally facial paralysis.
While acoustic neuromas don’t directly cause any change in oral health, the difficulties presented by facial paralysis and/or numbness can result in long-term oral complications. Facial paralysis often results in muscle weakness, which changes the way that patients eat, drink, talk, and smile. Facial paralysis can cause a myriad of unpleasant side effects, many of which pose a threat to maintaining good oral health. Often times individuals may bite the surface of their inner gums on the affected side, which can lead to ulcerations and infection. The lack of facial muscle control may also present challenges with activities that had previously been automatic, such as eating and drinking. It’s easy to take for granted the things that our bodies do on autopilot. The majority of people don’t have to worry about the way that their facial muscles are working while they enjoy a meal, but this can be a large source of anxiety for patients with facial paralysis. The physical motion of chewing and drinking can be difficult and result in drooling of saliva and food contents, which can be embarrassing. Eating and drinking in public is something that is so common, yet patients with facial paralysis often avoid it at all costs. This isolation over time can lead to negative changes in the patient’s mental and emotional frame of mind. To compensate, people with facial paralysis usually chew all of their food on the unaffected side of their mouth. While this may get the job done, it can result in jaw pain and disorders like temporomandibular joint dysfunction. Patient education, facial reanimation surgery, neuromuscular retraining, home dental hygiene (brushing and flossing), routine dental examination and periodontal appliances may be necessary to avoid long-term complications in the oral cavity.
Dry mouth can also be a side effect after the surgery and/or radiation therapy. Saliva plays an important role for the health of oral cavity. Saliva prevents root decay, cracked lips, rough tongue, bad breath and most importantly reduces the risk of infection on the tongue, cheeks and gums. To treat dry mouth, dentists may recommend mouth rinses that have fluoride and apply fluoride varnishes during the dental visits. Over the counter medications such as Biotine may also help some patients. Sugar-free gum, sugar-free hard candies and ice chips can also help relieve dry mouth. It is always recommended for patients to avoid carbonated drinks, caffeine, alcohol and tobacco and use of lanolin-based lip balm to help moisturize their dry lips.
Sometimes, acoustic neuroma patients experience trigeminal issues (or numbness) following surgery. This can exponentially increase the side effects of facial paralysis and dry mouth syndrome. When we eat, it’s common for small pieces of food to get stuck between the gums and cheeks. For the average person, this is not a problem because they have sensation of the food, and can use their tongue to dislodge it. When a patient with oral numbness has this experience, they will not notice the food. If left unattended, this can lead to major tooth decay. Furthermore, biting of inner gums may not be noticed, therefore leading to even more severe ulcerations and infections. As a result, it is even more important for this group of individuals to schedule regular dental exams, as there are additional threats to their oral health.
In summary, there are many important considerations that both patients and dentists should take into account when dealing with acoustic neuromas. Dentist should play a role as a member of the team of experts who treat acoustic neuroma patients. Educating acoustic neuroma patients about how facial paralysis or trigeminal nerve dysfunction can affect their oral health is of the upmost importance. Home dental hygiene such as brushing and flossing as well as routine dental exams should be encouraged for people who have had surgery or radiation therapy. Dentists should also be able to discern which cranial nerves were affected and use this information to help customize a treatment plan for their patients. When armed with the proper information, patients can make a conscious effort to schedule regular dental exams and maintain good oral health. If you are located in the Los Angeles area, we recommend Katrin Azizzadeh, DDS, who has special expertise in dental care for patients with facial paralysis.
References:
Whitaker E, Luchetti C. Treating The Oral Sequelae Of An Acoustic Neuroma. JADA 1996; 127:231-233.
Contact the Facial Paralysis Institute Today
If you have an acoustic neuroma and are struggling with the effects of facial paralysis and/or poor eyelid closure, contact Dr. Azizzadeh right away. His advanced surgical techniques may be able to restore some facial movement and put a smile back on your face! Call Dr. Azizzadeh at the Facial Paralysis Institute at (310) 657-2203 today to schedule a consultation.
To learn more about acoustic neuroma, contact our Beverly Hills office.
Request your consultation with Dr. Azizzadeh today
Call us at (310) 657-2203 to schedule an appointment.
Schedule a Consultation