Facial nerve anatomy is a key consideration relative to facial muscle movement and coordination. If facial nerve CN VII stops performing as expected, it can have far-flung effects on a person’s ability to smile, frown, and make other facial expressions.
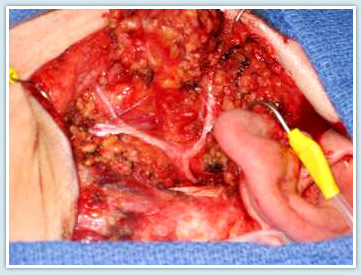
Photograph of facial nerve during a facial nerve preserving parotidectomy for benign parotid tumor (pleomorphic adenoma). This surgery was performed by Drs. Azizzadeh and Larian with the Facial Paralysis Institute.
An In-Depth Look at the Facial Nerve Anatomy of CN VII
The facial nerve resembles a telephone cable. It contains 7,000 individual nerve fibers, and each fiber carries electrical impulses to a specific facial muscle. Information passing along the fibers of this nerve allows people to laugh, cry, smile, or frown. That’s why facial nerve CN VII is commonly referred to as “the nerve of facial expression.”
When at least half of these individual nerve fibers are interrupted, facial weakness occurs. If these fibers are irritated, movements of the facial muscles appear as spasms or twitching.
Photograph of the facial nerve during a facial nerve preserving parotidectomy for benign parotid tumor (pleomorphic adenoma). This surgery was performed by Drs. Azizzadeh and Larian with The Facial Paralysis Institute.
The facial nerve not only carries nerve impulses to the muscles of the face, but also to the tear glands, saliva glands, and muscle of the stirrup bone in the middle ear (the stapes). It also transmits taste from the front of the tongue. The function of the facial nerve is complex, and many symptoms can occur when nerve fibers are disrupted.
CN VII Facial Nerve Disorder Symptoms
The facial nerve anatomy is extensive, and symptoms of a nerve disorder can vary. A disorder of the facial nerve can result in twitching, weakness, or paralysis of the face, dryness of the eye or mouth, and/or disturbance of taste. These symptoms can range in terms of onset and severity based on the extent of nerve damage and other factors.
An individual’s facial nerve passes through the base of the skull in transit from the brain to the muscles of facial expression. After leaving the brain, the facial nerve enters the bone of the ear (temporal bone) through a small bony tube (the internal auditory canal) in close association with the hearing and balance nerves.
Along its 1.5-in. course through a small canal within the temporal bone, the facial nerve winds around the three middle ear bones, behind the eardrum. The nerve then travels through the mastoid (the bony area behind the part of the ear that is visible).
After the facial nerve leaves the mastoid, it passes through the salivary gland in the face (parotid gland) and divides into branches that support various facial muscles. Facial nerve branches extend through the temporal bone to the tear gland, stapes muscle, tongue (for taste sensation), and saliva glands.
The facial nerve exits the skull behind the ear at stylomastoid foramen and enters the core of a salivary gland in front of the ear (parotid gland). Meanwhile, the parotid gland divides into an upper and lower division. It further divides into five main branches: the frontal, zygomatic, buccal, marginal mandibular, and platysmal.
There is arborization of facial nerve branches and significant variations that exist. Here is a look at major types and percentages of a facial nerve branching and anastomoses.
-
- In 13% of patients, major divisions (temporal and facial) are independent.
- In 11%, anastomoses occur between rami of the temporal division.
- In 22%, connections occur between adjacent rami from the major divisions.
- In 21%, anastomoses representing a composite of those in the 11% and 22% categories occur.
- In 12%, proximal anastomoses occur within the temporal component, as well as distal interconnection between the latter and the cervical component.
- In 9%, two anastomotic rami connect the buccal division of the cervical to the zygomatic part of the temporal.
- In 5%, a transverse ramus, from the trunk of the nerve, contributes to the buccal ramus formed by anastomosis between the two major divisions.
- In 7% richly plexiform communications occur, especially within the temporal portion of the nerve.
Variations of the facial nerve can also include branches that pass through clefts in superficial veins or the formation nerve loops through which pass superficial veins. Regardless of why these variations occur, they should be evaluated and treated appropriately. That way, people dealing with facial nerve disorders can treat such issues before they cause serious harm.
How Does Dr. Azizzadeh Treat a Facial Nerve Anatomy Disorder?
People who experience facial disorder symptoms should consult with an experienced facial plastic and reconstructive surgeon like Dr. Babak Azizzadeh of The Facial Paralysis Institute. This ensures an individual can work with a facial nerve anatomy expert to receive insights into their facial paralysis symptoms and why they are occurring. From here, Dr. Azizzadeh can determine if his patient is dealing with a Bell’s palsy CN VII disorder or other forms of facial paralysis.
Bell’s palsy CN VII symptoms can occur without notice. Common Bell’s palsy symptoms include temporary facial weakness or paralysis. These symptoms generally last for a few days or weeks and disappear on their own.
In instances where Bell’s palsy symptoms linger for an extended period of time, in-depth treatment options should be explored. Bell’s palsy symptoms can occur due to severe facial nerve CN VII damage. If the symptoms go undiagnosed and untreated, they can cause permanent facial paralysis. They can also result in facial asymmetry that hampers an individual’s appearance long into the future.
Dr. Azizzadeh can meet with a patient dealing with Bell’s palsy or other facial paralysis symptoms. At this time, he evaluates his patient’s facial appearance and symptoms. Dr. Azizzadeh can conduct several tests to analyze the severity of his patient’s symptoms.
The ideal treatment for a facial nerve disorder depends on the patient. In some instances, Dr. Azizzadeh recommends Botox to correct facial asymmetry without surgery. At other times, he recommends selective neurolysis or other surgical procedures.
With Botox, Dr. Azizzadeh relaxes unwanted muscle movements on the non-paralyzed side of his patient’s face. Botox injections can be administered in minutes and deliver results that can last up to four months. They help patients improve facial symmetry and alleviate facial paralysis symptoms.
Comparatively, Dr. Azizzadeh can perform selective neurolysis to permanently address facial nerve paralysis symptoms. During a selective neurolysis procedure, Dr. Azizzadeh releases the platysma muscle that pulls down the corner of the mouth. This helps a patient regain the ability to make natural facial expressions once again.
Dr. Azizzadeh works diligently to ensure his patient can achieve the best results from a non-surgical or surgical facial nerve disorder treatment. He may also recommend treatment be performed in combination with neuromuscular retraining, so his patient can improve facial muscle strength, movement, and coordination.
Explore Facial Nerve Disorder Treatment Options
There is no telling when facial nerve disorder symptoms will occur. But, these symptoms should be identified and treated in their early stages to minimize the risk of long-lasting facial paralysis.
Dr. Azizzadeh provides a wide range of facial nerve disorder treatments. Those who are suffering from facial paralysis or any other related condition can meet with Dr. Azizzadeh to assess myriad treatment options.
For more information or to schedule a consultation with Beverly Hills facial paralysis expert Dr. Azizzadeh, contact us online or call us today at (310) 893-6192. Also, read more about treatment of nerve injuries or nerve transplants.
NERVE INJURY
Request your consultation with Dr. Azizzadeh today
Call us at (310) 657-2203 to schedule an appointment.
Schedule a Consultation