Cranial nerve 7 palsy occurs when the facial nerve becomes damaged or inflamed, leading to weakness or paralysis of facial muscles. Its sudden onset not only affects physical expressions like smiling or closing the eyes but also carries emotional and social impacts for patients.
Key Takeaways
- Cranial nerve 7 palsy affects the seventh cranial nerve, causing facial muscle weakness or paralysis
- Bell’s palsy accounts for 60-75% of all facial nerve paralysis cases and often resolves on its own
- Symptoms include facial drooping, eye closure difficulty, and loss of taste on the affected side
- Early corticosteroid treatment within 72 hours significantly improves recovery outcomes
- Most patients recover completely, though some may experience long-term complications like synkinesis
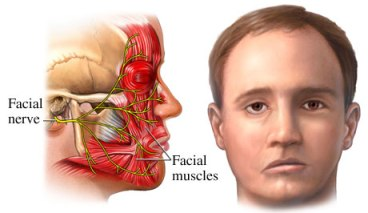
The Anatomy Behind Facial Nerve Function
The seventh cranial nerve is remarkably complex, originating deep in the brainstem and traveling through the temporal bone before branching out to control facial structures. It manages three primary functions: motor control of facial expression muscles, parasympathetic regulation of tear and saliva production, and sensory transmission of taste from the front of the tongue.
Because of its long, intricate pathway, the nerve is vulnerable to injury at multiple points, with damage in different locations producing distinct symptom patterns that guide diagnosis and treatment.
Understanding this anatomy explains why patients with facial paralysis and nerve disorders often experience seemingly unrelated symptoms like dry eyes alongside facial weakness.
Bell’s Palsy: The Most Common Form
Bell’s palsy dominates the landscape of cranial nerve 7 disorders, affecting approximately 40,000 Americans annually. This condition appears without warning, typically developing over 24 to 48 hours, leaving one side of the face completely or partially paralyzed.
What sets Bell’s palsy apart:
- Rapid onset without identifiable cause
- Usually affects only one side of the face
- Often preceded by ear pain or sensitivity to sound
- Associated with changes in taste perception
- Most cases begin recovering within 3-4 weeks
The exact cause remains mysterious, though researchers suspect viral infections may trigger an inflammatory response that compresses the facial nerve within its bony canal. Herpes simplex virus, Epstein-Barr virus, and varicella-zoster virus have all been implicated as potential triggers.
https://facialparalysisinstitute.com/blog/overcoming-the-effects-of-facial-paralysis-2
Recognizing the Symptoms
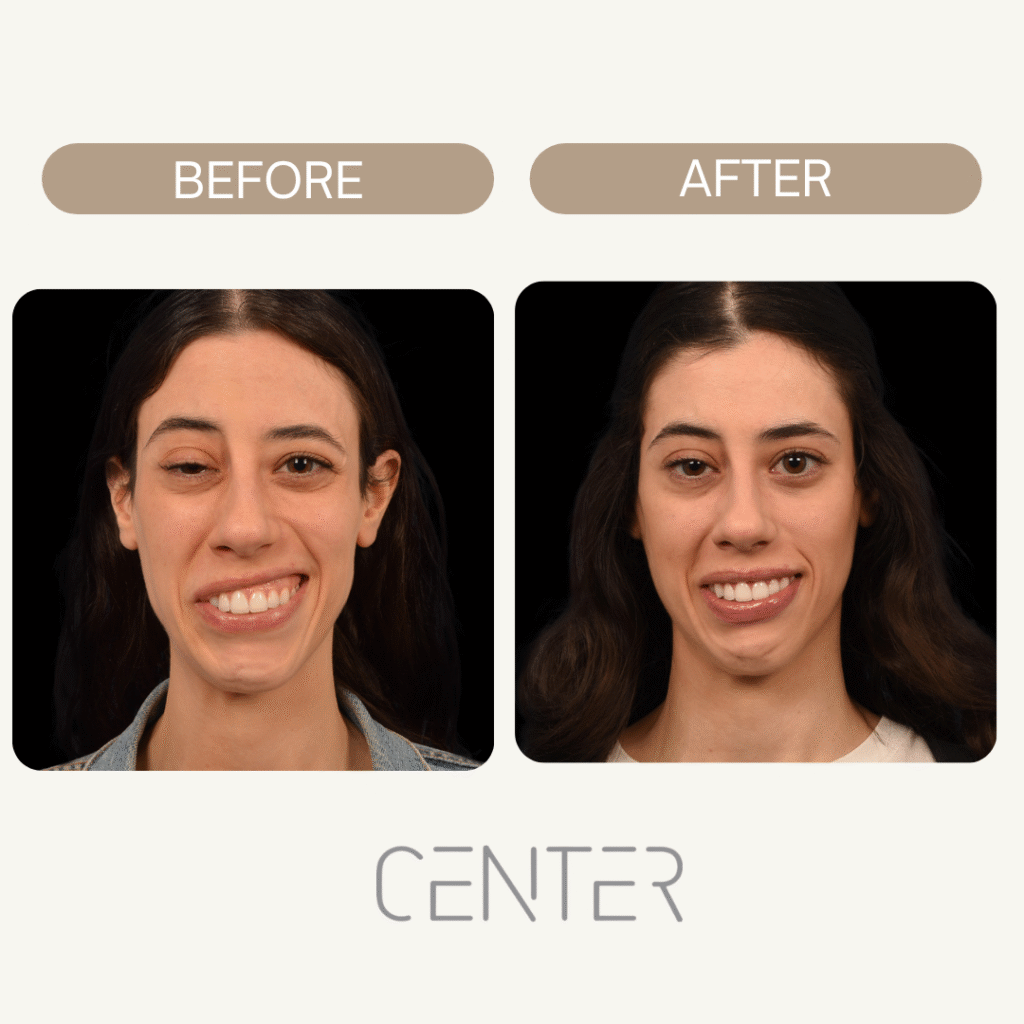
Cranial nerve 7 palsy presents with a distinctive pattern of symptoms that typically develop on one side of the face. The severity can range from mild weakness to complete paralysis, depending on the extent of nerve damage.
Primary symptoms include:
- Facial drooping – The affected side of the face appears to sag or droop
- Eye closure problems – Inability to fully close the eye on the affected side
- Smile asymmetry – The mouth pulls to one side when attempting to smile
- Forehead paralysis – Loss of ability to raise the eyebrow or wrinkle the forehead
- Taste alterations – Decreased or altered taste sensation on the front of the tongue
Secondary complications may develop:
- Excessive tearing or dry eyes
- Drooling due to poor lip closure
- Difficulty eating or drinking
- Slurred speech
- Increased sensitivity to sound (hyperacusis)
The House-brackmann Facial Paralysis Scale provides a standardized method for measuring the degree of facial nerve dysfunction, helping doctors track recovery progress and plan appropriate treatments.
Causes Beyond Bell’s Palsy
While Bell’s palsy represents the majority of cases, cranial nerve 7 palsy can result from numerous underlying conditions. Understanding these causes helps guide treatment decisions and predict recovery outcomes.
Infectious causes:
- Lyme disease
- Herpes zoster (shingles)
- Middle ear infections
- Meningitis
Traumatic causes:
- Skull fractures
- Surgical complications
- Birth trauma
Neoplastic causes:
- Acoustic neuromas
- Parotid gland tumors
- Meningiomas
Other medical conditions:
- Stroke affecting the brainstem
- Multiple sclerosis
- Sarcoidosis
- Diabetes mellitus
Each underlying cause may require specific treatment approaches beyond standard facial nerve rehabilitation. This is why proper bell’s palsy diagnosis involves ruling out these secondary causes through careful history-taking and appropriate testing.
Diagnostic Approaches
Diagnosing cranial nerve 7 palsy typically begins with a thorough clinical examination. Physicians assess facial symmetry, muscle strength, and associated symptoms to determine the extent and likely cause of the nerve dysfunction.
Standard diagnostic steps:
- Clinical history – Onset timing, associated symptoms, recent illnesses
- Physical examination – Facial movement testing, reflex assessment
- Neurological evaluation – Comprehensive cranial nerve testing
Additional testing may include:
- Blood tests to screen for Lyme disease or diabetes
- MRI scans to identify tumors or structural abnormalities
- Electrodiagnostic studies to assess nerve function
- Audiometry if hearing problems are present
Treatment Options and Management
Early intervention plays a crucial role in optimizing recovery from cranial nerve 7 palsy. Treatment approaches vary depending on the underlying cause, severity of symptoms, and timing of presentation.
Immediate medical management:
Corticosteroids represent the gold standard for Bell’s palsy treatment when started within 72 hours of symptom onset. These anti-inflammatory medications help reduce nerve swelling and improve recovery rates significantly.
Antiviral medications show limited benefit for Bell’s palsy, though they’re sometimes prescribed in combination with steroids. The evidence supporting their use remains controversial among medical professionals.
Eye protection measures:
- Artificial tears to prevent corneal drying
- Eye patches during sleep
- Protective glasses during daytime
- Regular ophthalmologic monitoring
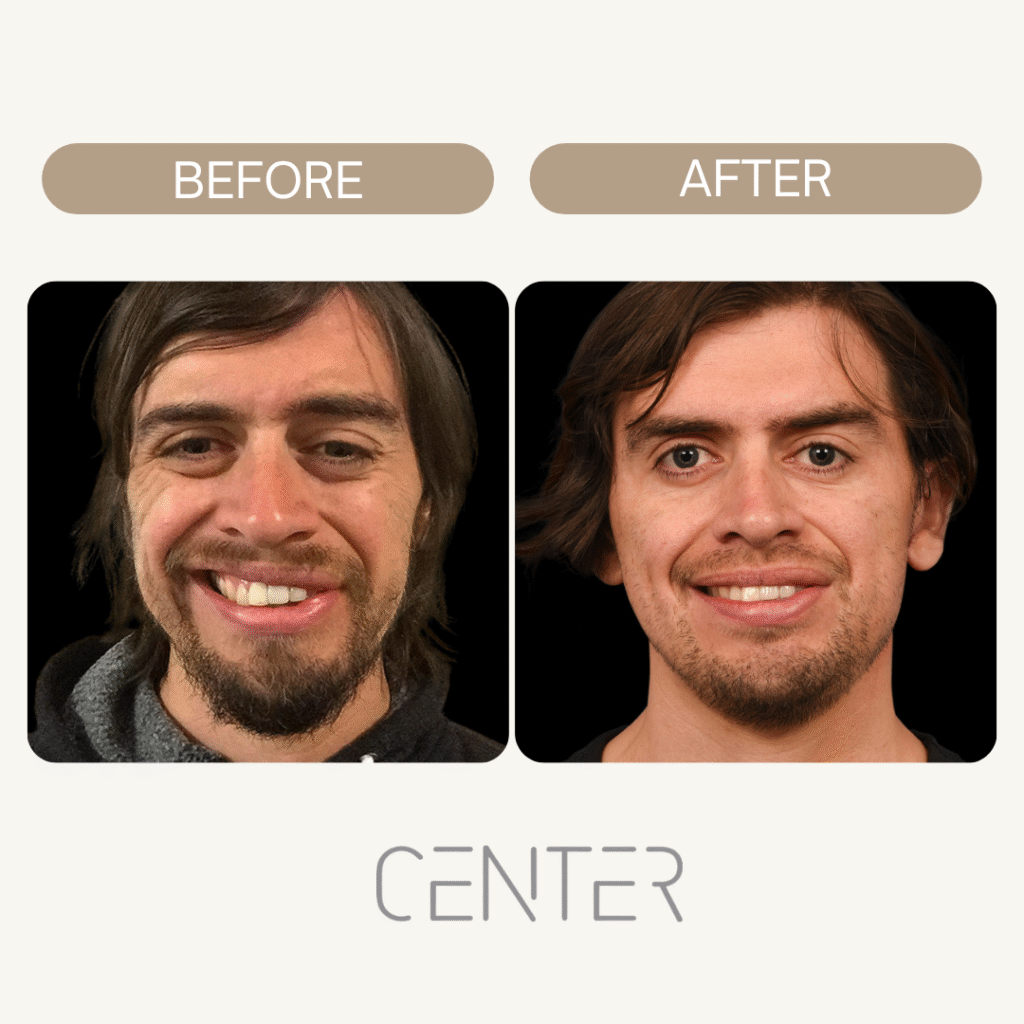
Physical therapy interventions:
Specialized expert-approved facial exercises can help maintain muscle tone and promote nerve regeneration. These exercises should be performed under professional guidance to avoid developing abnormal movement patterns.
Recovery and Prognosis
The recovery timeline for cranial nerve 7 palsy varies significantly based on the underlying cause and severity of nerve damage. Understanding what to expect helps patients maintain realistic expectations while staying motivated during rehabilitation.
Recovery patterns for Bell’s palsy:
- 85% of patients show some improvement within 3 weeks
- 80% achieve complete or near-complete recovery
- Most improvement occurs within the first 6 months
- Recovery after 12 months is less likely
Factors influencing recovery:
- Age at onset (younger patients typically recover better)
- Severity of initial paralysis
- Presence of other medical conditions
- Speed of treatment initiation
Some patients may experience incomplete recovery, leading to long-term complications such as synkinesis (involuntary muscle movements), facial contractures, or persistent weakness. Ongoing bell’s palsy management strategies can help address these issues.
Complications and Long-term Considerations
While most patients with cranial nerve 7 palsy recover well, some may develop complications that require ongoing attention and specialized bell’s palsy treatment approaches.
Common complications include:
Synkinesis – This involves involuntary facial movements that occur when trying to move other facial muscles. For example, the eye might close when attempting to smile.
Facial contractures – Permanent muscle tightening can develop, causing the affected side of the face to appear pulled or distorted.
Crocodile tears syndrome – Abnormal nerve regeneration can cause tears to flow when eating, as fibers intended for salivation mistakenly connect to the tear glands.
Persistent weakness – Some degree of facial weakness may remain permanently, affecting smile symmetry and facial expression.
Prevention and Risk Factors
While many cases of cranial nerve 7 palsy cannot be prevented, understanding risk factors can help with early recognition and prompt treatment.
Known risk factors include:
- Diabetes mellitus
- Pregnancy (especially third trimester)
- Upper respiratory infections
- Family history of Bell’s palsy
- Age between 15-45 years
Preventive measures:
- Prompt treatment of ear infections
- Good control of diabetes
- Protection from extreme cold weather
- Early treatment of viral infections
If you or a loved one is experiencing sudden facial weakness, learning about available care options is the first step toward recovery. Visit our page on Bell’s palsy treatment to explore expert-recommended therapies, discover when to seek specialist care, and find guidance tailored to your unique needs.
Conclusion
Cranial nerve 7 palsy, most often presenting as Bell’s palsy, causes sudden facial paralysis that can be alarming but usually improves with early treatment. Most patients recover fully, and for those with lingering symptoms, targeted therapies and supportive strategies can restore function and quality of life.
Request your consultation with Dr. Azizzadeh today
Call us at (310) 657-2203 to schedule an appointment.
Schedule a Consultation