Bell’s palsy and stroke are medical conditions commonly associated with facial paralysis. However, Bell’s palsy and stroke are not identical, and proper diagnosis is key to ensure safe, effective treatment of either condition. To better understand the differences between Bell’s palsy and stroke, let’s examine both conditions in detail.
When facial weakness strikes suddenly, distinguishing between these two conditions becomes critical. While both can cause alarming facial symptoms, their underlying causes, treatment approaches, and long-term outcomes differ significantly. This comprehensive guide breaks down everything you need to know about Bell’s palsy versus stroke, helping you recognize warning signs and understand when to seek immediate medical attention.
Understanding Bell’s Palsy: Causes and Characteristics
Bell’s palsy is a form of temporary facial paralysis that affects the seventh cranial nerve; this nerve is located in the skull and travels beneath the ears to muscles on both sides of the face. It causes an interruption in messages between the brain and facial nerves, resulting in facial paralysis or weakness.
When Bell’s palsy occurs, the seventh cranial nerve’s functionality is disrupted. This makes it difficult for an individual to open and close the eyes and smile, frown and make other facial expressions.
Key Bell’s Palsy Statistics
Bell’s palsy affects approximately 40,000 Americans annually, according to the National Institute of Neurological Disorders and Stroke (NIH). The condition impacts men and women at equal rates, and people above the age of 60 and under the age of 15 are less susceptible to Bell’s palsy than others.
Risk Factors for Bell’s Palsy
While the exact cause remains unknown, certain factors increase your risk:
- Pregnancy, especially during the third trimester
- Diabetes doubles your risk according to Mayo Clinic research
- Recent upper respiratory infections
- Family history of Bell’s palsy
- Compromised immune system
Psychosocial Impact of Bell’s Palsy
Sudden facial paralysis affects far more than muscle function. For many patients, especially teenagers and young adults, the visible changes can create deep social and emotional challenges. Everyday interactions like smiling, eating in public, or participating in conversations may feel daunting.
According to the National Institutes of Health, individuals with Bell’s palsy face a higher risk of developing anxiety and depression due to these changes in appearance and communication.
Adults in professional settings often report reduced confidence during meetings or presentations, while adolescents may struggle with peer relationships and self-esteem. Understanding this psychosocial dimension underscores why early diagnosis, treatment, and supportive counseling are so critical for recovery.

Bell’s Palsy Symptom Timeline
Bell’s palsy symptoms range from mild to severe, and they can affect one or both sides of the face. Common Bell’s palsy symptoms include facial twitching and weakness, along with facial paralysis. Additionally, people who experience Bell’s palsy are prone to:
- Drooling
- Eye or mouth dryness
- Excessive tearing
- Drooping at the eyelid and corner of the mouth
- Impaired taste
Oftentimes, Bell’s palsy symptoms reach their apex within 48 hours of onset. At this point, an individual coping with Bell’s palsy could experience:
- Ringing in one or both ears (tinnitus)
- Headache
- Impaired speech
- Dizziness
- Hypersensitivity to sound
- Difficulty eating or drinking
The 72-Hour Window
Research from the National Institute of Neurological Disorders shows that most Bell’s palsy patients experience peak symptoms within 72 hours. This rapid progression distinguishes it from other conditions that cause gradual facial weakness over weeks or months.
Medical Associations with Bell’s Palsy
To date, no known cause of Bell’s palsy has been identified. There is an understanding that Bell’s palsy occurs due to inflammation that affects the seventh cranial nerve, yet research is ongoing to determine the precise cause of this inflammation. Meanwhile, Columbia University Department of Neurology notes that Bell’s palsy symptoms are sometimes associated with a variety of medical conditions, including diabetes, high blood pressure and Lyme disease.
Understanding Stroke: A Vascular Emergency
In comparison to Bell’s palsy, stroke is a leading cause of disability and the fifth-ranked cause of death in the United States, American Stroke Association (ASA) states. Stroke refers to a disease that impacts arteries in the brain.
It occurs when a blood vessel that transports oxygen and nutrients to the brain is blocked; this blockage happens due to a clot or bursts. In this instance, the brain cannot get the necessary blood and oxygen it needs to function properly, thus resulting in the death of brain cells.
Types of Strokes
Ischemic Stroke (87% of all strokes)
An ischemic stroke occurs when a blood vessel that supplies blood and oxygen to the brain is obstructed; this type of stroke accounts for roughly 87% of all strokes, ASA reports.
Warning signs specific to ischemic stroke
Patients should be alert to these hallmark symptoms:
- Sudden numbness or weakness, especially on one side of the body
- Confusion or difficulty speaking
- Vision problems in one or both eyes
- Severe headache with no known cause
Hemorrhagic Stroke (13% of all strokes)
A hemorrhagic stroke takes place when a weakened blood vessel ruptures, which causes blood to accumulate in the brain and compress surrounding brain tissue. ASA points out that hemorrhagic strokes account for about 13% of all strokes.
Unique hemorrhagic stroke symptoms
This type of stroke often presents with sudden, dramatic warning signs, including:
- Sudden, explosive headache (often described as a “thunderclap”)
- Nausea and vomiting
- Stiff neck
- Sensitivity to light
Transient Ischemic Attack (TIA) – “Mini Stroke”
A TIA, also called a mini stroke, refers to a temporary blockage of blood flow to the brain. Although a TIA likely won’t cause permanent damage, it could be a warning sign that a full-blown stroke could occur in the foreseeable future, ASA states.
Critical TIA Facts from the American Stroke Association
- About 40% of people who experience a TIA will go on to have an actual stroke
- Nearly half of all strokes occur within days of a TIA
- Symptoms usually last less than 5 minutes, but in some cases can persist up to 24 hours
Brain Impact: Left vs Right Hemisphere
Ultimately, a stroke can affect both the left and right sides of the brain.
Left Brain Stroke Effects
- Paralysis on the right side of the body
- Speech problems, aphasia
- Memory loss
- Cautious, slow behavior
Right Brain Stroke Effects
- Paralysis on the left side of the body
- Vision problems
- Memory loss
- Quick, impulsive behavior
Bell’s Palsy vs Stroke: Critical Symptom Differences
Quick Comparison Table
| Bell’s Palsy | Stroke |
|---|---|
| Affects facial nerve only | Affects brain tissue |
| Facial weakness develops over hours or days | Symptoms appear within minutes |
| Usually affects the entire side of the face | May affect only the lower face |
| No arm or leg weakness | Often includes limb weakness |
| Can wrinkle forehead on affected side | Cannot wrinkle forehead if upper face is involved |
| No confusion or speech problems | May include confusion or slurred speech |
| Pain behind ear is common | Sudden severe headache possible |
Detailed Symptom Analysis
In patients dealing with Bell’s palsy, the seventh cranial nerve becomes inflamed. The nerve’s branches control motor and sensory functions of the cheeks, mouth, eyelids, and tear glands. As such, Bell’s palsy can affect a patient’s ability to salivate, frown, and perform other facial muscle movements relating to these functions.
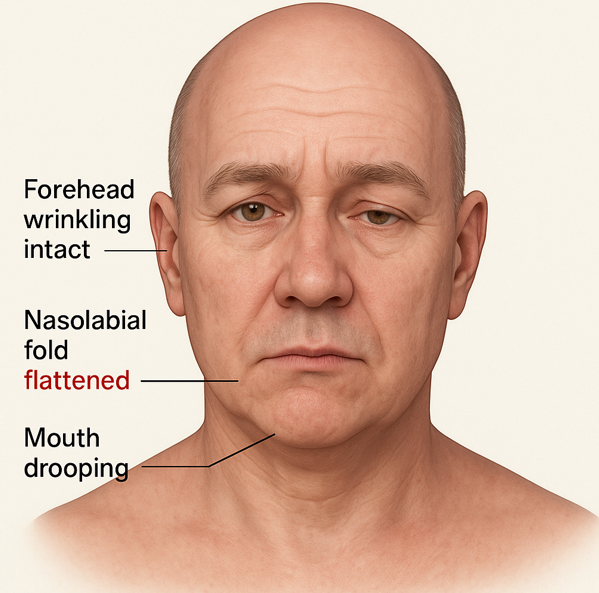
With Bell’s palsy, facial weakness can occur in a peripheral pattern in which the forehead mouth, eye, and forehead are affected. Bell’s palsy can hinder a patient’s ability to:
- Grimace or smile
- Open or close the eye
- Lift or furrow their eyebrow
- Control tear production
It can also cause flattening of the nasolabial fold.
During a stroke, a patient experiences an abrupt disruption in the delivery of oxygen and nutrients to the brain. The symptoms of a stroke can appear within minutes of the disruption and vary based on the affected blood vessel and the resulting shortage of oxygen and nutrients in the brain.
A stroke can cause central facial weakness in which only the mouth is affected. But, there may also be times when strokes result in facial weakness that affects the mouth, eye, and forehead. In these cases, other focal neurologic deficits may be present as well.
The F.A.S.T. Test for Stroke Recognition
According to the CDC’s stroke guidelines, the FAST test helps quickly identify stroke symptoms:
- Face drooping: Ask the person to smile. Is it uneven?
- Arm weakness: Can they raise both arms equally?
- Speech difficulty: Is speech slurred or unusual?
- Time: If any of these symptoms are present, call 911 immediately.
Proper assessment of a patient’s symptoms is vital in cases where facial weakness has occurred. By undergoing a neurological examination and other testing, patients can find out if they are dealing with Bell’s palsy or stroke.
Professional Assessment: Bell’s Palsy vs Stroke

A Bell’s palsy patient can display unilateral facial paralysis that replicates a stroke. The patient can also experience reduced tearing, drooping on the paralyzed side of the face, slurred speech, and other symptoms.
Along with symptoms commonly associated with Bell’s palsy, a stroke patient can experience:
- Dizziness
- Loss of coordination
- Changes in vision
- Other sensory issues
Most stroke patients can also blink the eyes and furrow the brow.
Emergency Room Evaluation Process
If patients display symptoms of Bell’s palsy or stroke, doctors use a structured assessment to provide an accurate diagnosis. The evaluation typically involves:
Initial Assessment
A doctor’s initial assessment involves reviewing a patient’s medical history and performing a physical exam. They also monitor vital signs and establish a timeline of symptom onset.
- Medical history review
- Physical examination
- Vital signs monitoring
- Timeline of symptom onset
Neurologic Examination
The neurologic exam allows a doctor to examine a patient’s level of consciousness and their ability to perform facial muscle movements. It can include:
- Cranial nerve exam
- Stroke scale evaluation (NIH Stroke Scale)
- Reflex testing
- Sensation assessment
- Coordination tests
Following testing, a doctor determines a safe, effective way to help a patient manage their symptoms. The doctor can use the insights to properly diagnose Bell’s palsy or stroke and help a patient achieve long-lasting symptomatic relief.
Advanced Diagnostic Tools
While clinical examination is the starting point, advanced testing provides greater accuracy and insight:
- Electromyography (EMG): Evaluates electrical activity in facial muscles to determine severity and location of nerve damage in Bell’s palsy.
- Magnetic Resonance Imaging (MRI): With contrast, reveals subtle inflammation around the facial nerve and helps rule out other neurological conditions.
- Computed Tomography (CT) Angiography: Identifies blockages or abnormalities in blood vessels associated with stroke.
- Multidisciplinary Evaluation: Collaboration between neurologists and facial nerve specialists ensures comprehensive assessment, reduces diagnostic delays, and improves long-term treatment outcomes.
Diagnostic Testing and Treatment Approaches
For an individual who displays any signs of facial paralysis or stroke, immediate diagnosis and treatment is essential. By meeting with a doctor at the first sign of Bell’s palsy or stroke symptoms, an individual can get the help necessary to address these symptoms.
Bell’s Palsy Diagnosis
There are no laboratory tests used to diagnose Bell’s palsy, according to NIH. Instead, a doctor examines a patient to assess any signs of upper and lower facial weakness.
Diagnostic tests may include:
- Electromyography, EMG, to verify nerve damage
- Blood tests for diabetes, infections, and other conditions
- MRI or CT scan to identify structural issues
- Neurologic assessment
- Hearing test
- Tearing test
- Ear, nose, and throat evaluation
Stroke Diagnosis
ASA states that a doctor performs two types of tests to diagnose stroke:
Imaging Tests
- MRI scans
- CT scans
- These help identify the stroke’s cause, its location, and the extent of the brain injury.
Blood Flow Tests
- Cerebral angiography
- These evaluate blood flow through vessels, detecting blockages and assessing their severity.

Treatment Options
Bell’s Palsy Treatment Progression
Once a doctor diagnoses Bell’s palsy, initial treatment usually involves:
- High-dose steroids (prednisone)
- Antiviral medications
If a Bell’s palsy patient does not respond to this treatment, other treatment options are available:
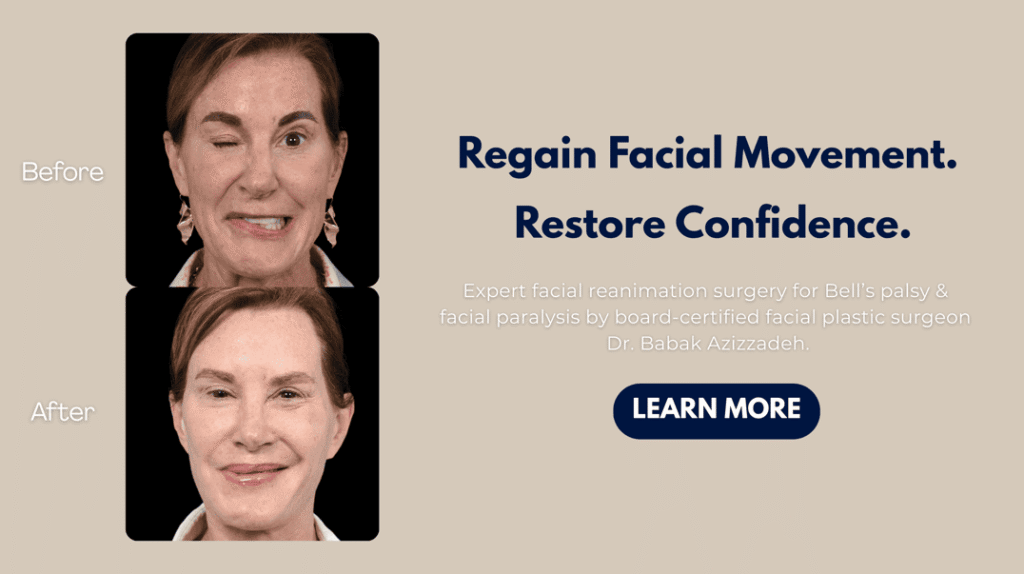
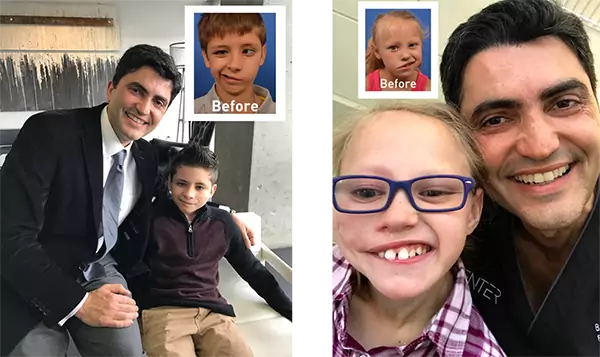
Selective Neurolysis: Developed by globally recognized facial plastic and reconstructive surgeon Dr. Babak Azizzadeh, selective neurolysis is a surgical procedure that helps Bell’s palsy patients achieve a natural-looking smile.
Botox: Bell’s palsy patients can receive Botox injections that temporarily restore facial symmetry and improve the facial appearance.
“Supercharging” Procedure: A “supercharging” or “signal upgrading” surgical procedure helps increase the power of the facial nerve and strengthen weak smile muscles.
Rehabilitation After Stroke
Recovery does not end with acute stroke treatment. Rehabilitation plays an essential role in helping patients regain lost abilities and adapt to long-term changes. Stroke rehabilitation typically involves a multidisciplinary team, including physical therapists to restore movement and balance, occupational therapists to rebuild daily living skills, and speech-language pathologists to improve speech and swallowing.
The American Stroke Association emphasizes that patients who begin rehabilitation within 48 hours of their stroke often experience significantly better functional outcomes. Beyond regaining independence, early and consistent rehabilitation also helps reduce the risk of secondary complications such as muscle contractures, pneumonia, or falls. This comprehensive approach ensures patients achieve the highest possible quality of life following a stroke.
Physical Therapy Options
Studies from peer-reviewed research show that facial exercises can significantly improve recovery outcomes when started early. These exercises help maintain muscle tone, support nerve regeneration, and prevent long-term complications such as contractures.
Stroke Treatment by Type
Stroke treatment varies based on the type of stroke, ASA states.
Ischemic Stroke Treatment
- Tissue plasminogen activator (r-tPA) within 4.5 hours
- Endovascular procedures
- Mechanical thrombectomy to remove blood clots
Hemorrhagic Stroke Treatment
- Endovascular procedures to stop bleeding
- Surgery to secure blood vessels at aneurysm base
- Blood pressure management
TIA Treatment
- Anti-platelet drugs
- Anticoagulants
- Thrombolytic agents
- Endarterectomy for fatty deposit removal
- Angioplasty to open clogged arteries
The Bottom Line on Bell’s Palsy vs Stroke
If a patient displays symptoms of facial weakness or paralysis, there is no need to wait to pursue medical treatment. At this time, a doctor can assess a patient to find out if their symptoms are related to Bell’s palsy or stroke. The doctor can then provide the patient with a personalized diagnosis and treatment plan.
Patients who fail to address their Bell’s palsy or stroke symptoms risk long-term health problems. By being proactive in their efforts to manage these symptoms, patients can alleviate facial weakness and other issues before they escalate. These patients can also take the necessary steps to prevent facial paralysis from hampering their ability to smile, frown, and make other natural facial expressions.
[INFOGRAPHIC: Bell’s Palsy vs Stroke – already exists, keep embed code]
Long-Term Outlook and Prevention
The long-term outlook varies depending on whether paralysis stems from Bell’s palsy or stroke. Most Bell’s palsy patients recover fully within months, and recurrence is rare. In contrast, stroke survivors must take proactive steps to reduce the risk of another event.
Preventive measures include managing high blood pressure, controlling diabetes, exercising regularly, and following a heart-healthy diet. Ongoing medical follow-up is essential to monitor progress and maintain neurological health.
For patients dealing with persistent facial weakness, specialists such as Dr. Azizzadeh provide advanced reconstructive procedures that not only restore function but also enhance quality of life, helping individuals return to work, social activities, and family life with renewed confidence.
Schedule a Facial Paralysis Treatment Consultation with Dr. Azizzadeh Today
Why Choose Dr. Azizzadeh for Facial Paralysis Treatment
Dr. Babak Azizzadeh is an internationally recognized leader in facial paralysis treatment. His credentials include:
- Harvard-trained facial plastic and reconstructive surgeon
- Director of the Facial Paralysis Institute
- Pioneer of the selective neurolysis technique
- Author of more than 100 peer-reviewed articles on facial nerve disorders
- Featured expert on The Oprah Winfrey Show and The Doctors
- Named one of the “Best Doctors in America”
Facial paralysis is a problem that affects both Bell’s palsy and stroke patients. With help from Dr. Azizzadeh, a Bell’s palsy or stroke patient can quickly and safely address his or her facial paralysis symptoms.
Dr. Azizzadeh is a Harvard-trained facial plastic and reconstructive surgeon with many years of facial paralysis treatment experience. He works closely with each patient to understand his or her facial paralysis symptoms and delivers a custom treatment plan. That way, Dr. Azizzadeh can help Bell’s palsy and stroke patients correct their facial paralysis symptoms.
Patient Success Rate
Dr. Azizzadeh’s innovative surgical techniques have helped thousands of patients regain facial function. For appropriate surgical candidates, success rates exceed 90%, according to published outcomes data.
Dr. Azizzadeh is available to meet with a Bell’s palsy or stroke patient to explore facial paralysis treatment options. To schedule a facial paralysis treatment consultation with Dr. Azizzadeh, please contact us online or call us today at (310) 657-2203.
[DEV NOTE: Add CTA button here: “Schedule Your Consultation Today”]
Request your consultation with Dr. Azizzadeh today
Call us at (310) 657-2203 to schedule an appointment.
Schedule a Consultation