The parotid gland sits just in front of and below each ear, and running directly through it is one of the body’s most delicate structures: the facial nerve. This nerve controls everything from your smile to your ability to blink, which is why any surgery involving the parotid gland requires exceptional precision.
Key Takeaways
- The facial nerve passes through the parotid gland, making preservation a top priority during tumor removal.
- Advanced intraoperative monitoring allows surgeons to track nerve activity throughout the procedure.
- Most patients experience temporary weakness rather than permanent damage when treated by experienced specialists.
- Surgeon expertise and technique directly impact outcomes in facial nerve preservation surgery.
- Immediate nerve repair options exist for complex cases where the nerve cannot be fully preserved.
Understanding the Facial Nerve’s Role
The facial nerve branches into five main divisions after exiting the skull, each controlling different regions of the face. These branches govern your ability to raise your eyebrows, close your eyes, smile, and move your lower lip. When Facial Nerve Disorders occur, the effects can range from subtle asymmetry to complete paralysis on one side of the face.
Because the facial nerve runs directly through the parotid gland, any tumor growing in this area poses a potential threat to normal facial function. The goal of Parotidectomy With Facial Nerve Preservation is to remove the tumor completely while keeping every branch intact and functioning.

https://facialparalysisinstitute.com/blog/rehabilitation-of-central-facial-paralysis
Why Preservation Matters
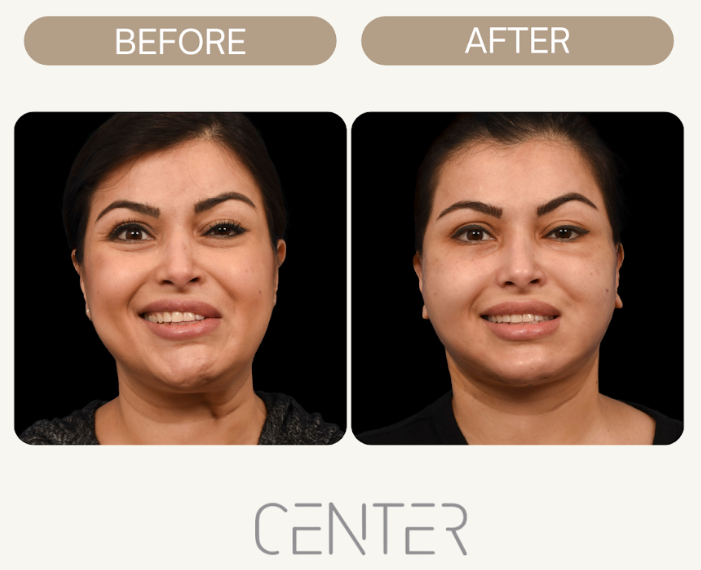
Facial movement is something most people take for granted until it’s compromised. The ability to smile at loved ones or simply close your eyes while sleeping depends entirely on proper facial nerve function. Research on facial nerve preservation during parotid surgery shows that outcomes depend heavily on the surgeon’s experience and techniques.
Temporary facial weakness after parotidectomy is relatively common, even with careful nerve preservation. This typically resolves within weeks to months as the nerve recovers from gentle manipulation during surgery. Permanent damage occurs far less frequently when the procedure is performed by a specialist with extensive experience.
The Surgical Approach
Modern parotidectomy relies on meticulous dissection and real-time nerve monitoring. Here’s what the process typically involves:
- Preoperative Imaging: MRI or CT scans help the surgical team understand the tumor’s exact location and relationship to the facial nerve.
- Intraoperative Monitoring: Small electrodes placed in the facial muscles detect nerve activity throughout surgery. When the surgeon approaches a nerve branch, the monitoring system alerts the team.
- Careful Dissection: The surgeon identifies the main trunk of the facial nerve and traces each branch, gently separating the tumor from surrounding nerve tissue.
- Tumor Removal: Once all nerve branches are identified and protected, the tumor and necessary portions of the parotid gland are removed.
Understanding the risks of parotidectomy helps patients make informed decisions and set realistic expectations.

https://facialparalysisinstitute.com/blog/the-anatomy-of-a-smile-and-facial-synkinesis
Signs of Facial Nerve Injury
Recognizing facial nerve injury symptoms early allows for prompt intervention. Common indicators include weakness or drooping on one side of the face, difficulty closing the eye, asymmetry when smiling, and changes in taste sensation.
If symptoms persist beyond the expected recovery period, Facial Nerve Decompression Surgery can relieve pressure on a damaged nerve and promote healing.
Factors That Influence Outcomes
Several factors affect the likelihood of successful nerve preservation:
- Tumor Location: Superficial lobe tumors are generally easier to remove without nerve damage than deep lobe tumors, which sit closer to nerve branches.
- Tumor Size: Larger tumors require more extensive dissection and may have grown into or displaced the facial nerve.
- Benign vs. Malignant: Cancerous tumors sometimes invade the facial nerve directly, making complete preservation impossible in certain cases.
The Role of Surgeon Expertise
Experience matters tremendously in facial nerve preservation. Surgeons who perform high volumes of parotid procedures develop the refined technique needed to handle complex cases safely.
Dr. Babak Azizzadeh is recognized internationally for his expertise in facial nerve surgery and restoration. His work in facial paralysis treatment has advanced techniques for both nerve preservation and reconstruction, giving patients access to sophisticated care.
When Preservation Isn’t Possible
In rare cases involving aggressive cancers that have invaded the facial nerve, complete preservation may not be achievable. When this happens, immediate nerve reconstruction becomes the priority. Techniques including nerve grafting can restore some degree of facial function, though results vary based on the extent of damage.
The decision to sacrifice any portion of the facial nerve is never taken lightly. It’s made only when necessary to achieve complete tumor removal.
If you’re facing parotid surgery and want to explore your options with a team dedicated to preserving facial function, request a consultation to discuss your case in detail.
Conclusion
Facial nerve preservation parotidectomy represents the intersection of technical skill and compassionate patient care. With advanced monitoring technology, refined surgical techniques, and specialists who dedicate their practice to these procedures, most patients can expect excellent outcomes and preserved facial function.
Frequently Asked Questions
How long does facial weakness last after parotidectomy? Most temporary weakness resolves within two to six months. The timeline varies based on the extent of nerve manipulation during surgery.
Can the facial nerve be repaired if it’s damaged during surgery? Yes. Immediate nerve grafting techniques can restore function in many cases, though recovery takes time and results depend on the severity of the injury.
What should I look for when choosing a parotid surgeon? Seek a surgeon with extensive experience in parotid procedures, access to intraoperative nerve monitoring, and a track record of successful outcomes.
Will I have a visible scar after parotidectomy? Incisions are typically placed in natural skin creases around the ear to minimize visibility. Most scars fade significantly over time.
Is facial nerve monitoring standard for all parotidectomies? At specialized centers, yes. Nerve monitoring has become the standard of care and reduces the risk of permanent nerve injury.
Request your consultation with Dr. Azizzadeh today
Call us at (310) 657-2203 to schedule an appointment.
Schedule a Consultation