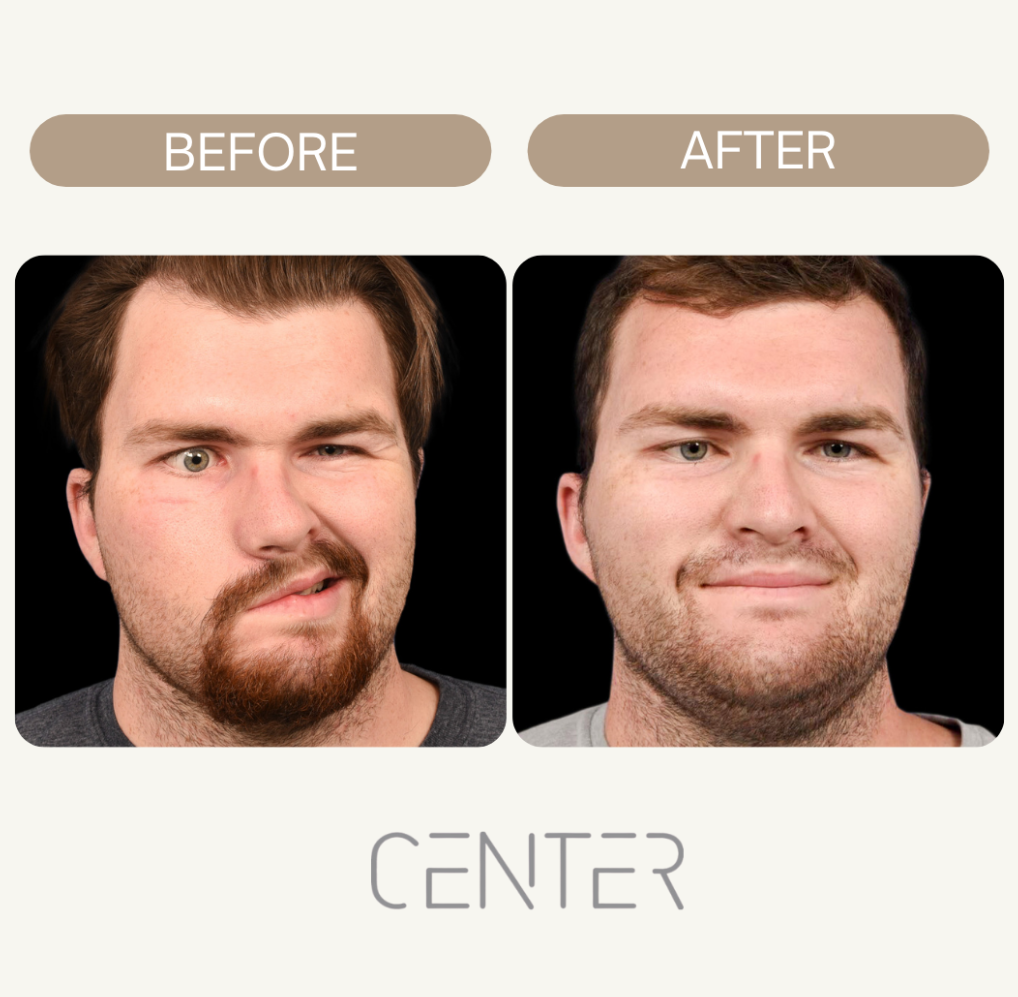
Facial paralysis can be a tough thing to deal with. It can mess with how you look and even how you do everyday stuff, like eating or blinking. But good news! There are operations, called Facial Reanimation Surgery Explained, that can really help. These procedures aim to get some movement back in your face or at least make things look more even. It’s a big step, but for many, it makes a huge difference in their lives.
Understanding Facial Reanimation Surgery Explained
What is facial reanimation surgery? Basically, it’s a set of procedures designed to restore movement and symmetry to your face if you’ve experienced facial paralysis. It’s not just about looks; it’s about getting back functions like smiling, blinking properly, and even speaking clearly. The goal is to improve your quality of life by addressing both the aesthetic and functional impacts of facial paralysis.
The Imperative for Surgical Intervention
Why even consider surgery? Well, facial paralysis can really mess with your life. It can affect your self-esteem, make it hard to communicate, and even cause physical problems like dry eye. Sometimes, physical therapy and other treatments aren’t enough, and that’s where surgery comes in. It’s about weighing the potential benefits against the risks and deciding if it’s the right path for you.
Distinguishing Static and Dynamic Procedures
There are two main types of facial reanimation surgery: static and dynamic. Static procedures are all about improving symmetry when your face is at rest. Think of them as providing support and structure. Dynamic procedures, on the other hand, aim to restore actual movement. They might involve nerve grafts or muscle transfers to get your face moving again. Here’s a quick breakdown:
- Static: Improves symmetry at rest.
- Dynamic: Restores facial movement.
- Both can be used in combination for optimal results.
Choosing between static and dynamic procedures, or a combination of both, depends heavily on the specifics of your condition, the extent of the paralysis, and your personal goals. It’s a conversation you’ll have with your surgeon to determine the best approach.
Static Procedures: Restoring Facial Symmetry
When facial paralysis strikes, it can throw your whole face off balance. Static procedures are all about bringing back that symmetry, even if they don’t restore movement. Think of them as the foundational work before any dynamic, movement-focused surgeries.
Eyelid Procedures for Ocular Protection
One of the biggest concerns with facial paralysis is protecting the eye. If you can’t fully close your eyelid, your eye can dry out, leading to serious problems. Eyelid procedures are designed to address this. A common one involves placing a small weight, often gold or platinum, in the upper eyelid. This helps the lid close more completely, protecting the eye from damage and dryness.
- Upper eyelid weight placement
- Lower lid tightening
- Tarsal strip procedure
Facelift Techniques for Enhanced Balance
A facelift isn’t just for wrinkles; it can play a key role in restoring symmetry after facial paralysis. The paralyzed side of the face tends to droop over time, making it look older than the unaffected side. A facelift tightens the skin and underlying tissues, lifting the face and creating a more balanced appearance. It’s like hitting the reset button on the effects of gravity and nerve damage. Consider facial suspension to improve facial symmetry.
The Role of Static Slings
Static slings are another way to provide support and lift to the paralyzed side of the face. These slings, often made of fascia lata (a strong tissue from your own body) or synthetic materials, are surgically placed to lift the corner of the mouth or other areas that have drooped. They act like internal scaffolding, providing immediate improvement in facial symmetry. Static slings offer a structural solution, counteracting the effects of muscle weakness. A fascia lata sling can help improve symmetry at rest.
Static procedures are often the first step in facial reanimation. They address immediate concerns like eye protection and facial asymmetry, laying the groundwork for more complex, movement-restoring surgeries down the line. They’re about bringing back balance and confidence, even before movement is fully restored.
Dynamic Procedures: Reanimating Facial Movement
Static procedures can help with symmetry, but dynamic procedures? That’s where we start talking about getting actual movement back. It’s a whole different ballgame, and it involves some pretty amazing techniques. It’s not just about looks; it’s about function – smiling, blinking, all those little things we take for granted.
Nerve Grafting and Transfer Techniques
Neurografts are like circuit rewiring. Sometimes a damaged nerve blocks the signal. To bridge the gap, surgeons use a nerve from another part of the body, usually a less critical one. Nerve transfer involves rerouting a functioning nerve to power face muscles. Slow, but effective, it can restore natural movement. Not immediately, though. The final results may take months or a year. Let your nerves do their thing and be patient. The success depends on a number of factors, including:
- The extent of the nerve damage
- The patient’s age
- The time since the injury occurred
Muscle Transposition and Transfer
If nerves are injured or muscles are atrophied, muscle transposition or transfer may work. Take a leg or chewing muscle and move it to the face. A surgeon meticulously joins blood vessels and nerves so the muscle can function in its new location. Complex, yet crucial to face movement restoration. It’s crazy to use a muscle for anything else.
The Significance of Temporalis Muscle Transfers
The temporalis muscle, one of the muscles you use to chew, is a popular choice for facial reanimation. It’s close by, and it’s powered by a different nerve than the facial nerve, so it’s often still working even when the facial nerve is damaged. The surgeon can detach part of the temporalis muscle and re-route it to the corner of the mouth. This allows you to smile by clenching your jaw. It takes some getting used to, but it can provide a really significant improvement in facial expression. Eyelid procedures for ocular protection are also important to consider.
Advanced Nerve Reconstruction Techniques
Cross-Facial Nerve Grafting
Cross-Facial nerve grafting involves grafting healthy nerves to paralyzed side to create a bridge for nerve signals, aiming for a more natural smile, with results taking up to a year.
Hypoglossal-Facial Anastomosis
Hypoglossal-Facial Anastomosis connects the facial nerve to the hypoglossal nerve, controlling tongue movement and facial muscles. While not a perfect solution, it can restore some facial movement.
Nerve to Masseter Muscle Transfer
The nerve to masseter muscle transfer connects the facial nerve, triggering a smile when the jaw is clenched, albeit not a natural smile.
Hypoglossal-Facial Anastomosis
Hypoglossal-Facial Anastomosis connects the facial nerve to the hypoglossal nerve, controlling tongue movement, aiming to restore facial movement, but may be a trade-off for some individuals.
Nerve to Masseter Muscle Transfer
The nerve controlling the masseter is connected to the facial nerve, triggering a smile when the jaw is clenched, resembling learning a new facial language.
Note: The success of nerve reconstruction depends on the extent of nerve damage, overall health, and the surgeon’s skill.
The Surgical Journey: What to Anticipate
Embarking on facial reanimation surgery is a significant decision, and understanding what lies ahead can ease anxiety and promote a smoother experience. Let’s walk through what you can expect, from the initial consultation to the first stages of recovery.
Pre-Surgical Evaluation and Planning
• Thorough evaluation of the patient’s medical history, physical exam, and imaging tests.
• Creation of a personalized plan outlining different surgical options and realistic results.
Anesthesia and Operative Considerations
• Most facial reanimation surgeries are performed under general anesthesia.
• The length of the surgery can vary, with simple procedures taking a few hours and complex reconstructions taking longer.
• The surgical team prioritizes patient safety and comfort.
Post-Operative Care and Recovery
• Post-surgery, close monitoring, pain management, and hospital stay are key.
• Detailed instructions on care for the surgical site, medication, and avoidance of activities are provided.
• Recovery times vary, but patience and careful follow-up are crucial.
Here’s a general idea of what the recovery timeline might look like:
- First few days: Expect swelling, bruising, and some discomfort.
- First few weeks: Focus on wound care and pain management.
- Several months: Gradual return of muscle function, with ongoing physical therapy.
Innovations in Facial Reanimation Surgery Explained
Facial reanimation surgery is undergoing significant advancements, with surgeons using smaller incisions, advanced imaging, and robotics to improve precision and reduce recovery time. These new approaches aim to provide more natural and symmetrical results, allowing quicker return to daily life.
Advancements in Muscle Transfer Techniques
Muscle transfer is a key part of dynamic facial reanimation. Instead of using the whole muscle, surgeons are now using smaller portions or even just the tendon, like in temporalis tendon transfer. This can lead to more controlled and natural movements. Also, research is being done on using artificial muscles to restore facial movement. This could be a game-changer for people who don’t have suitable muscles for transfer.
Future Directions in Facial Paralysis Treatment
The future of facial reanimation is looking bright. Here are a few areas that are showing promise:
- Gene Therapy: Researchers are exploring ways to use gene therapy to stimulate nerve regeneration and muscle growth.
- Stem Cell Therapy: Stem cells could potentially be used to repair damaged nerves and muscles in the face.
- 3D Printing: Custom implants and scaffolds could be 3D printed to support facial structures and improve surgical outcomes.
These innovations are not just about restoring movement; they’re about improving quality of life. The goal is to help you regain confidence and reconnect with the world through a natural and expressive smile.
It’s an exciting time for facial reanimation surgery, with new technologies and techniques constantly emerging to improve outcomes and patient experiences.
Want to know more about how we’re making big strides in helping people with facial paralysis? Our website has all the details on the newest ways we’re doing facial reanimation surgery. Come check it out!
Wrapping It Up
Facial reanimation surgery is a complex area, with lots of different ways to help people get back some movement and symmetry in their faces. Whether it’s fixing nerves, moving muscles around, or doing some cosmetic tweaks, the goal is always to make things better for folks dealing with facial paralysis. It’s a big deal for them, and these surgeries can really change lives.
Request your consultation with Dr. Azizzadeh today
Call us at (310) 657-2203 to schedule an appointment.
Schedule a Consultation