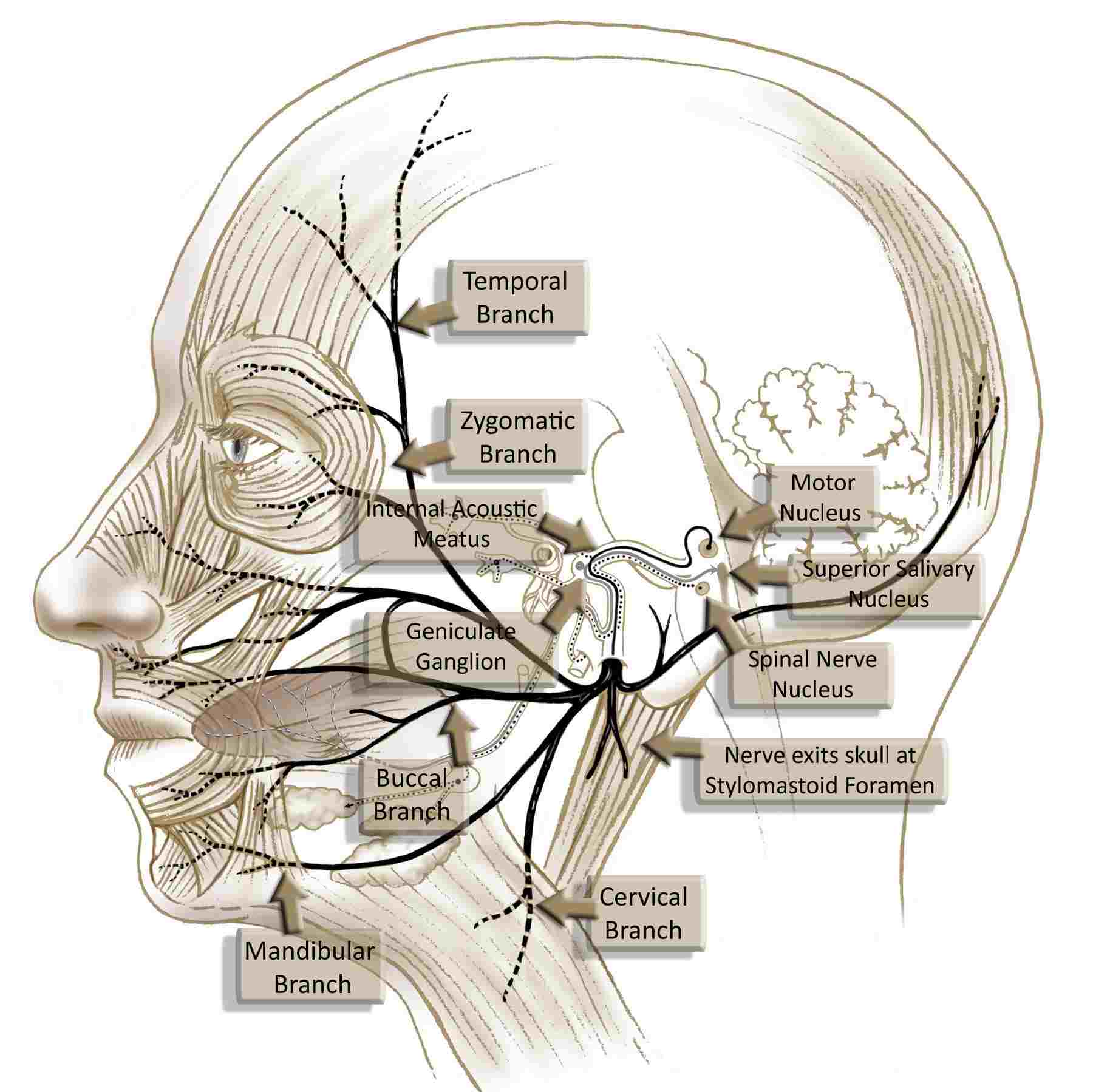
In patients with long-term facial paralysis who are older than 55, cross-facial nerve grafts have not produced great results. Dr. Babak Azizzadeh, a world-renowned facial plastic and reconstructive surgeon, takes an alternative approach to treat long-term facial paralysis in these patients. He utilizes the hypoglossal nerve or trigeminal nerve as the neural supply for the gracilis muscle transplant (see gracilis muscle section).
The nerve of the gracilis muscle is attached to the hypoglossal nerve in the neck; the hypoglossal nerve is responsible for moving the tongue muscle. By using hypoglossal facial nerve transfer and attaching a partial portion of the nerve to the transplanted gracilis muscle, a patient can extend their tongue to voluntarily move their face.
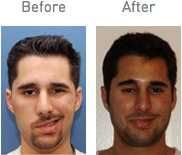
This state-of-the-art procedure can improve facial muscle movement in patients coping with long-term facial paralysis. And, it helps these patients achieve a natural facial appearance. (Source: Dr. B. Azizzadeh, Facial Paralysis Institute)
The facial nerve controls the muscles responsible for smiling, blinking, and other expressions. When this nerve is damaged, patients may experience complete or partial paralysis on one side of the face. Hypoglossal-facial nerve transfer surgery works by redirecting nerve fibers from the tongue to the paralyzed facial muscles, allowing new pathways for movement to develop over time. This technique has been refined over decades and remains one of the most effective options for patients who are not candidates for other nerve grafting procedures.
Do You Qualify for a Hypoglossal Nerve Procedure?
Patients can qualify for a hypoglossal nerve transfer if they have experienced facial paralysis symptoms for a minimum of two years. Also, the trigeminal nerve must work correctly for a patient to qualify for a hypoglossal facial nerve transfer procedure.
The hypoglossal canal through which the hypoglossal nerve can play a key role in a patient’s eligibility for a nerve transfer. Patients must have a trigeminal nerve that functions properly to qualify for treatment. But, damage to the hypoglossal canal can affect the nerve and reach a point where it is tough for patients to swallow, speak, and make other muscle movements that involve the tongue. In these instances, patients can consider a gracilis free tissue transfer or other hypoglossal facial nerve transfer treatment options.
According to research on hypoglossal-facial nerve anastomosis, patients who undergo the procedure within the first 12 months of paralysis onset tend to experience stronger outcomes. However, for older patients or those with longer-term paralysis, this technique remains one of the most reliable options available. The cause of paralysis also plays a role in determining candidacy. Patients whose facial nerve damage resulted from tumor removal, trauma, or viral conditions like Bell’s palsy may all be considered for this procedure after a thorough evaluation.
During your consultation, Dr. Azizzadeh will assess several factors to determine if hypoglossal-facial nerve transfer is right for you. These include the health of your remaining facial muscles, the condition of the donor nerve, and your overall medical history. Patients with certain health conditions or those who have had previous surgeries in the area may require alternative approaches, which is why a personalized evaluation is so important.
Related: Gracilis Muscle Transplant
How Is a Gracilis Free Tissue Transfer Used?
The primary use of gracilis free tissue transfer in the head and neck region is in the form of a muscular free flap for the dynamic rehabilitation of long-standing permanent facial paralysis. When combined with cross-facial nerve grafting or used as a single-stage reconstruction, free tissue transfer offers the best prospect for restoring spontaneous emotional facial expression.
Benefits of this muscle over other free flaps used for dynamic facial reanimation include consistent anatomy with large caliber vessels, ease of harvest, a 2-team approach, reliability, and acceptable donor site morbidity.
Drawbacks of hypoglossal facial nerve transfer include excessive bulk, skin tethering, and a donor site scar that may be minimized with minimally invasive techniques. Secondary procedures to refine the results are often necessary to achieve a good final result.
Ultimately, the choice of muscle for dynamic facial reanimation depends on the surgeon’s experience and comfort level. (Source: Jason H Kim, MD, Assistant Professor, Department of Otolaryngology-Head and Neck Surgery, University of California at Irvine http://www.emedicine.com/ent/ext709.htm)
Some patients may also benefit from masseter-facial nerve transfer, which uses the nerve controlling the chewing muscle instead. The best approach depends on each patient’s anatomy, the cause of their paralysis, and their treatment goals.
Comparing Treatment Options: Hypoglossal vs. Gracilis Free Tissue Transfer
Evaluate multiple options for treatment of Bell’s palsy and other forms of facial paralysis. This allows a patient coping with facial paralysis to gain insights into different treatment options. Next, the patient can find an appropriate treatment, regardless of whether he or she is dealing with a rare condition that causes their facial paralysis symptoms.
A hypoglossal-facial nerve transfer or gracilis free tissue transfer can be used to treat facial paralysis. However, the safety and efficacy of each treatment depends on the patient, the severity of their facial paralysis symptoms, and other factors.
One common intervention is facial reanimation surgery, which helps restore expression through a variety of techniques. A nerve transplant for facial paralysis may also be recommended depending on the patient’s unique circumstances and the duration of their condition.
Dr. Azizzadeh can perform an evaluation to patients who have been dealing with facial paralysis symptoms for eight months or longer. He can provide a personalized treatment recommendation designed to help a patient alleviate their facial paralysis symptoms.
Plus, he can craft a hypoglossal-facial nerve transfer treatment plan that limits the risk of damage to the carotid arteries or other complications. This ensures a patient can receive a treatment to restore their ability to smile, frown, and produce other natural facial expressions and improve their facial appearance.
Why Choose Dr. Babak Azizzadeh? As a dual board-certified facial plastic surgeon with fellowship training in facial nerve disorders, Dr. Azizzadeh has dedicated his career to helping patients with facial paralysis. His experience with complex nerve transfer procedures and commitment to individualized care make him a trusted choice for patients seeking lasting results.
What to Expect During Recovery
Healing after a hypoglossal–facial nerve transfer happens in stages and takes time. During the early postoperative period, it’s common to have localized swelling and soreness near the incision, which usually improves with prescribed pain control and adequate rest.
Many patients are able to resume basic everyday tasks within a couple of weeks, but activities that place physical strain on the body, including intense workouts or lifting heavy objects, are typically restricted for several more weeks.
The real progress begins around the five to six month mark, when patients start to notice the first signs of facial tone returning. This happens as the regenerating nerve fibers reach the facial muscles and begin to establish new connections. Over the following months, voluntary movement gradually improves. Many patients find that working with a facial rehabilitation therapist during this time helps them maximize their results and learn to control their new movements more naturally.
It’s worth noting that the brain plays a significant role in recovery. Because the hypoglossal nerve originally controlled tongue movement, patients initially need to think about moving their tongue to activate their facial muscles. Over time, many patients develop more spontaneous, automatic movement as the brain adapts to the new nerve pathways. This process, called cortical plasticity, varies from person to person but continues to improve for up to two years after surgery.
Take the Next Step Toward Facial Restoration
If you’re living with facial paralysis and want to explore your options, schedule your personalized consultation with Dr. Azizzadeh today.
Summary
For most older patients, the hypoglossal nerve palsy treatment will cause less pain and have a shorter recovery time in comparison to many other treatment options. Over 95% of hypoglossal nerve transfer patients will experience some pain and minor complications but will also have great results with the surgery.
Hypoglossal-facial nerve transfer procedure is used on patients 55 years of age and older to limit postoperative trauma and speed up the recovery process. These patients can use the procedure to enhance their facial appearance, too. Yet, to achieve full facial reanimation, patients may require additional therapy and/or surgeries.
Frequently Asked Questions
How long does recovery take after hypoglossal-facial nerve transfer?
Most patients begin to notice improvements in facial tone within five to six months after surgery. Full results, including voluntary movement, may take 12 to 18 months as the nerve fibers regenerate and the brain adapts to the new pathways. Working with a facial rehabilitation specialist can help speed this process and improve overall outcomes.
Will I have trouble speaking or swallowing after the procedure?
Modern techniques use a partial hypoglossal transfer, which preserves most tongue function. While some patients experience mild, temporary changes in speech or swallowing, these typically improve with time and therapy if needed. Research shows that end-to-side and split anastomosis techniques significantly reduce tongue-related side effects compared to older methods.
What is the difference between hypoglossal and masseter nerve transfer?
Both procedures restore facial movement, but they use different donor nerves. Hypoglossal transfer uses the tongue nerve, while masseter transfer uses the chewing nerve. Hypoglossal transfer tends to produce excellent resting symmetry, while masseter transfer may offer faster recovery of smile function. Dr. Azizzadeh will recommend the best option based on your anatomy and goals.
How do I know which nerve transfer procedure is right for me?
The best procedure depends on several factors, including the cause and duration of your paralysis, the condition of your facial muscles, and your personal goals. Some patients benefit from a combination of techniques. During your consultation, Dr. Azizzadeh will conduct a comprehensive evaluation and discuss all available options so you can make an informed decision together.
Explore Facial Paralysis Treatment Options with Dr. Azizzadeh
If you are suffering from facial paralysis or a related condition, Dr. Azizzadeh can provide assistance. He offers free in-person and virtual consultations to people coping with long-term facial paralysis symptoms. To learn more about hypoglossal-facial nerve transfer or request a consultation, please contact The Facial Paralysis Institute online or call us today at (310) 657-2203.
NERVE TRANSPLANT- Cross Facial Nerve Graft
HYPOGLOSSAL FACIAL NERVE TRANSFER
Request your consultation with Dr. Azizzadeh today
Call us at (310) 657-2203 to schedule an appointment.
Schedule a Consultation